Human Rights and Mental Health Uruguay
Mental Disability Rights International
a project of the
Center for Human Rights & Humanitarian Law
Washington College of Law, American University
and the
Bazelon Center for Mental Health Law
Washington, D.C.
June 1995
Acknowledgements
MDRI is indebted to many people in Uruguay who took the time to offer MDRI their observations and insights. To protect their privacy, most of the individuals MDRI interviewed are not named in this report, including many people who use or reside in Uruguay's mental health facilities, members of their families, mental health service providers, members of psychiatric and nursing professional associations, representatives of the Uruguay Ministry of Public Health, the judiciary, and their staff.
MDRI's work in Uruguay would have been impossible without the invitation and assistance of the Instituto de Estudios Legales y Socia/es del Uruguay (IELSUR) and without the close collaboration and invaluable guidance of Francisco Ottonelli, Executive Director of IELSUR, and Sylvia Cousin, a member of IELSUR's Board of Directors. Thanks to the many staff members at IELSUR who arranged all aspects of the MDRI fact-finding mission in Uruguay and offered their open hospitality. Special thanks to Mariana Terra for her long hours of translation and for her warm, thoughtful, and thought provoking introduction to the history, culture, and sights of Uruguay. Christian Courtis, Legislative Aide in the Senate of Argentina, also provided valuable support as a translator and as an active member of the fact-finding mission in Uruguay.
Professor Herman Schwartz, Co-Director of Washington College of Law (WCL) Center for Human Rights and Humanitarian Law provided the support and vision that made the creation of MORI possible and that assured the success of the Uruguay project. Professor Robert Dinerstein of the Washington College of Law provided detailed comments on an early draft of this report. Professor Claire Morel-Seytoux of the University of Monterrey, Mexico, Karen Bower of the Women's Law & Public Policy Program at Georgetown University Law Center, and Melissa Crow, Schell Fellow at Human Rights Watch also contributed valuable comments on the draft. Thanks to Felipe Michelini of the Center for Justice and International Law (CEJIL/Sur), Montevideo, Uruguay, for advising MDRI on this project. Dr. Peter Statsny, Einstein Medical College, reviewed the report and contributed psychiatric references.
Angelica Moncada and Simon Abromovici conducted valuable background research on the mental health law of Uruguay. Peter Hansen helped proof the English text of the report. The report was translated into Spanish by Jerome V. Luhn, Laura Noriega-Martin, Alejandra Segura, and Professor Guillermo Ramirez, Laura Bergman, Valentina Delich, Monique Byrne, and Dr. Luis Byrn. Christian Courtis and Liliana Obregon painstakingly reviewed and prepared the final Spanish translation of the report for publication.
The Washington College of Law Center for Human Rights and Humanitarian Law funded the publication of this report. MDRI's work on the Uruguay project was funded by the Echoing Green Foundation, the Nathan Cummings Foundation, the Bazelon Center for Mental Health Law, and the Washington College of Law Center for Human Rights & Humanitarian Law. Clarence J. Sundram, Leonard S. Rubenstein, and the University of Miami School of Law generously contributed to the cost of travel and research in Uruguay.
Foreword
After centuries of indifference, human rights concerns are now recognized as essential to a free, democratic and humane society, of concern to all decent people everywhere. Because human rights issues arose originally in political contexts, primary emphasis has understandably been given to political rights like speech, press and association. The rights of institutionalized persons were of concern only if they were associated with political abuses.
That has changed somewhat, but the rights of the mentally disabled are still not on advocates' radar screens. Yet, if experience in the United States is any indication, few groups are subjected to as much discrimination, cruelty, and just sheer neglect and indifference. Only pretrial detainees are treated as badly, and as to them, there is at least a suspicion of wrongdoing, despite the presumption of innocence. People with mental disabilities are, however, completely innocent. The only crimes in which they are involved are those that are perpetrated upon them.
Nor is it likely that the United States is unique in this regard. Even in other free democratic societies like Uruguay, where the mental health workers are dedicated to humane treatment of the mentally disabled, this report finds that:
Conditions in Uruguay's psychiatric institutions violate a broad range of rights codified in the [United Nations Principles for the Protection of Persons with Mental Disabilities], including protections against harm and unjustified medica tion, respect for personal dignity, privacy and choice, and the right to treatment directed toward the preservation and enhancement of personal autonomy.
So little attention has been paid to these unlucky people, that despite international treaties, United Nations action, and other well-intentioned initiatives, human rights advocates know little about the treatment of the mentally disabled, and have done even less.
That must change. Those of us concerned about human rights must become aware of the inhumane treatment that even the most civilized societies inflict on the mentally disabled, and start doing something about it. This may be an especially auspicious moment for that, for there is increasing international interest in the treatment of the disabled, as reflected in Article 22 of the Declaration of the United Nations World Conference on Human Rights in Vienna in June 1993, and in the appointment of a U.N. Special Rapporteur on the Equalization of Opportunities for Persons with Disabilities.
This report by the Mental Disability Rights International project of the American University Human Rights Center on the treatment of the mentally disabled in Uruguay is a major step in that direction. It documents the combination of neglect, indifference and outright cruelty that is perpetrated on these helpless people in one country, and it charts a strategy for change that takes into account the economic and social situation in that country. It is indispensable reading for all who are concerned about what has been, until now, a dark corner of human rights abuse. With luck it will be just a beginning.
Professor Herman Schwartz
Executive Summary
This report documents human rights conditions in Uruguay's mental health system and recommends steps necessary to bring the system into conformity with internationally recognized human rights standards. The report is the product of a fact-finding mission conducted November 29 - December 8, 1993 by a Mental Disability Rights International (MDRI) team of attorneys and a psychiatrist. The team came to Uruguay at the request of the Instituto de £studios Legales y Socia/es de! Uruguay (IELSUR), a human rights group based in Montevideo, Uruguay.
The identification of human rights violations in this report should not detract from the impressive efforts of the individuals who work in Uruguay's mental health system who have devoted themselves to the care and concerns of people with mental disabilities. Nor should this report undervalue the strengths of Uruguay's mental health system, its great human resources, and the widespread interest in the rights of people with mental disabilities which together hold promise for Uruguay to be a leader in mental health system reform.
A. Structure of Services
The public mental health system of Uruguay relies almost exclusively on large in-patient institutions at the expense of community-based care. There are more than 2,000 people in Uruguay's public psychiatric institutions (from a total population of 3.1 million people) of whom 1,300 to 1,400 live in asylums (known as "Colonias") in remote parts of the country. Most patients in the Colonias remain there for life.
A few impressive public and private community mental health programs exist in Uruguay. Public programs serve fewer than 200 individuals, however, and they cannot accommodate the large numbers of people who need community services. By official accounts, one-half to two-thirds of people in Uruguay's mental health system are "social patients" without any need for psychiatric hospitalization.
Many "social patients" are not mentally ill but are detained in institutions because they happen to be homeless or have no place else to go. People are held in institutions for committing petty crimes, for alcoholism, epilepsy, old age, or mental retardation. Institutional ization of people with retardation in Uruguay's psychiatric facilities is particularly inappropriate and harmful, because these individuals receive no services tailored to their special needs.
Uruguay's medical and social service systems do not accommodate the needs of people with mental disabilities living in the community, creating added stress that leads to further institutionalization. Mental health coverage other than psychotropic medication is not included in mainstream health care. Disability pensions are terminated for people who obtain a job of any kind, even if such employment does not provide subsistence income.
In the mid-1980s, shortly after Uruguay's return to democracy, the Ministry of Public Health brought together a National Commission to study the need for mental health reform. The National Program for Mental Health put forward by the Commission in September 1986 recommended that Uruguay "abandon the hospital" as the primary locus of mental health services and develop community-based services integrated into the national health system. The National Program for Mental Health was adopted by the Ministry of Public Health, but funds were never allocated for its implementation.
Uruguay's near-exclusive reliance on institution-based treatment results in the unjustified, unnecessary, and potentially harmful institutionalization of people capable of safely living and working in the community. The structure of Uruguay's mental health system thus violates internationally accepted medical and human rights standards adopted by the Pan American Health Organization (PAHO) in the Declaration of Caracas, and the United Nations General Assembly in the Principles for the Protection of Persons with Mental Illness (Ml Principles). The detention of "social patients" at the discretion of hospital authorities constitutes arbitrary detention prohibited by the International Covenant on Civil & Political Rights (the ICCPR) and the American Convention on Human Rights (the American Convention). The improper and unjustified hospitalization of individuals capable of living in the community results in decreased social functioning and violates the right to the "highest attainable standard of ... mental health" protected by the International Covenant on Economic, Social, and Cultural Rights (ICESCR).
International law requires that the detention of "social patients" be terminated and community-based alternatives to psychiatric hospitals be established. Resources currently available for mental health care must be re-directed to ensure the enforcement of internationally recognized human rights. Uruguay is under a legal obligation to invest additional resources for mental health system reform, if this is necessary to enforce the full protections of the ICCPR and the American Convention. To bring Uruguay's mental health system into line with internationally accepted human rights standards, MDRI recommends that Uruguay:
A-1 End the detention of "social patients";
A-2 Conduct a system-wide review of all current commitments to psychiatric institutions;
A-3 Create community-based mental health care and other alternatives to psychiatric institutions;
A-4 Create services to allow people with mental retardation to live in the community;
A-5 End disincentives to work in pension benefits;
A-6 Include psychiatric coverage in mainstream health care.
With or without a further legislative mandate, Uruguay's Ministry of Public Health should:
A-7 Take a leadership role in restructuring the mental health system;
A-8 Involve system users and families in reform efforts;
A-9 Publicly present a plan to the legislature for implementing reforms, including a budget and a timetable.
The Ministry of Public Health's plan should estimate both the cost of creating services in the community and the savings that will arise from closing institutions. Uruguay may need to invest additional resources to restructure its mental health system, particularly to create community-based mental health services, and the implementation plan should include a realistic estimate of these new costs.
B. Civil Commitment
The civil commitment law of Uruguay (entitled the "Law of Assistance to Psychopaths") does not provide the minimum substantive or procedural protections required by the MI Principles.
Uruguayan law allows commitment upon medical certification (requiring the consent of an institution director, two physicians, and a relative). There is no requirement that a patient be dangerous or in need of psychiatric treatment. The only criterion for such commitment is a medical finding of "mental illness," a provision that is not enforced, since large portions of the patient population are not mentally ill. Uruguayan law does not provide a right to independent, periodic review of civil commitment, nor does it provide a right to counsel in commitment proceedings, as the MI Principles require.
On its face, the mental health law of Uruguay violates the minimum requirements of the MI Principles and the protections against arbitrary detention in the ICCPR and the American Convention. Thus, Uruguay must:
B-1 Revise the mental health law to include the establishment of proper substantive commitment standards and procedural protections (including a right to independent, periodic review of commitment, and a right to counsel in commitment proceedings) as required by the MI Principles.
C. Conditions in Institutions
For individuals committed to psychiatric institutions, the experience can be destructive rather than helpful. For most patients, psychiatric services do not enhance personal autonomy or support reintegration into the community. Treatment is often inappropriate and unnecessarily dangerous.
Psychiatric treatment in public institutions is almost totally limited to somatic therapies (psychotropic medications and electroconvulsive therapy (ECT)). These treatments are often administered with no medical justification, e.g. on individuals with mental retardation and no psychiatric diagnosis. The absence of complete treatment records, the lack of specific diagnoses, the shortage of professional staff, and the inadequate monitoring of side-effects render the safe and effective use of psychotropic medications impossible for many patients.
Psychiatric institutions provide no psychotherapy and little rehabilitation or vocational training. Only a minority of patients receive case management to assist them in returning to their work, family, and community. Thus, patients sleep or sit by their bedside, wander the halls, or do nothing most of the day. Whatever social and vocational skills they may have had upon entry are generally allowed to deteriorate.
Living conditions are generally not respectful of the dignity and privacy of residents.
With the exception of a few bed areas where patients have put up a photo or kept a stuffed animal, institutions are almost completely impersonal, undecorated, and drab. Many of the institutions are in old and decrepit buildings, and in some areas the conditions are unhygienic (e.g. the Colonia Etchepare security ward, where clogged toilets flood hallways and where some patients sleep on bare, filthy floors).
There is no system for protecting patients' rights in institutions, and important decisions concerning their rights (including transfer to some locked wards) are made at the discretion of administrators without standards, guidelines, or oversight. Although physical restraints and seclusion appear to be rarely used, there are no established regulations for their use. Some individuals are reported to be held in seclusion for four to six weeks.
Patients are not notified of their rights, and there is a general lack of recognition that they have rights. No complaint mechanisms have been established, nor are there any mechanisms to investigate allegations of abuse or violence.
International pharmaceutical manufacturers are reported to be testing new psychotropic medications in institutions with permission from Uruguayan authorities. MDRI is concerned about potential risks to patients and possible lack of safeguards, including the patients' informed consent, as required by the ICCPR.
Conditions in Uruguay's psychiatric institutions violate a broad range of rights codified in the Ml Principles, including protections against harm and unjustified medication, respect for personal dignity, privacy, and choice, and the right to treatment directed toward the preservation and enhancement of personal autonomy. Improper and dangerous treatment practices and conditions in Uruguay's mental health system unnecessarily and unjustifiably cause great suffering, violating the ICCPR and the American Convention's protections against inhuman treatment. In certain cases, conditions or treatment may be life-threatening, violating the right to life guaranteed by the ICCPR and the American Convention. Conditions leading to the deterioration of mental health and social functioning violate the right to enjoyment of the highest attainable standard of physical and mental health as guaranteed in the ICESCR.
To bring Uruguay's mental health system into conformity with international human rights standards, Uruguay should:
C-1 Adopt treatment standards, including procedures for the proper and safe use of psychotropic medications and ECT;
C-2 Ensure broad-based involvement in development of standards;
C-3 Refer to internationally accepted psychiatric practice guidelines;
C-4 Use internationally accepted diagnoses;
C-5 Improve treatment plans and records;
C-6 Establish a quality assurance system;
C-7 Implement treatment and service programs that build upon existing community supports;
C-8 Conduct a thorough review of current medication and ECT practices;
C-9 Investigate pharmaceutical marketing/research practices;
C-10 Establish continuing education requirements for staff;
C-11 Address problems of staff morale;
C-12 Attack public stigma and the pervasive problem of anomie (despair) in institutions.
D. Oversight
The Ministry of Public Health does not monitor treatment practices at public institutions, and the authorities report that there are no standards by which institutions can be assessed.
The only independent oversight of psychiatric institutions is provided by what is called the "Inspector General of Psychopaths, " a position that was vacant for twenty years. The new Inspector, who took office in October 1993, promised to review every psychiatric commitment in the country. He has only two professional staff members to support him. Patients do not have a right to participate in commitment reviews. Indeed, they may never know about the review, which may be-based solely on a telephone conversation between the Inspector and the institution director.
The government of Uruguay is responsible under international human rights treaties to ensure the safety and well-being of patients detained in mental health facilities. Given the poor conditions in psychiatric facilities, the dangerous treatment practices, and the lack of proper safeguards in the civil commitment process, the existence of independent oversight is particularly important. MDRI recommends that Uruguay engage in a thorough review of treatment practices and:
D-1 Create an effective oversight mechanism to ensure the enforcement of rights in institutions;
D-2 Publicly report on conditions annually;
D-3 Establish human rights committees in psychiatric facilities;
D-4 Support consumer and family advocates.
E. Recommendations to Advocates and the International Community
To create political support for national mental health reform, advocates in Uruguay should:
E-1 Bring together a broad base of constituents for reform including system users, family groups, community providers, mental health professionals, and human rights advocates;
E-2 Re-establish momentum around Uruguay's 1985-86 National Reform Plan which called for the creation of community-based mental health care;
E-3 Educate the public about conditions in institutions and about the existence of alternatives to institutions.
The international community should press for the enforcement of international human rights law:
E-4 The United Nations Special Rapporteur on the Equalization of Opportunities for Persons with Disabilities should evaluate the conditions of people with mental disabilities in Uruguay and Uruguay's efforts to create services and programs that will provide people with mental disabilities the full opportunity to live and work community. The Special Rapporteur should provide technical assistance to Uruguay to create service programs in the community and should help raise international financial support for the development of such programs;
E-5 The United Nations Human Rights Committee should require Uruguay to report on the enforcement of rights of people with mental disabilities under the ICCPR;
E-6 The United Nations Committee on Economic, Social, and Cultural Rights should require Uruguay to report on the enforcement of rights of people with mental disabilities under the ICESCR.
Preface: Goals & Methods of this Report
Mental Disability Rights International (MDRI) sent a fact-finding team to Uruguay in November-December 1993 at the invitation of the Instituto de Estudios Legates y Socia/es del Uruguay (IELSUR), a human rights organization based in Montevideo active in advocating for the rights of people with mental disabilities in Uruguay. Long concerned with human rights violations in the mental health system, IELSUR is initiating a new effort to bring about major reforms in the mental health laws and services in Uruguay.
This report documents human rights conditions in Uruguay's mental health system and recommends steps necessary to bring the system into conformity with internationally recognized human rights standards. This report is the product of a fact-finding mission to Uruguay conducted from November 27 to December 9, 1993 by an inter-disciplinary team of four attorneys and a psychiatrist from the United States and an attorney from Argentina.1 Members of the MDRI team interviewed representatives of the Uruguay Ministry of Public Health, governmental and non-governmental service providers (institution and community program administrators, psychiatrists, social workers, nurses, and other staff), representatives of mental health professional organizations, the President of the Uruguay Supreme Court and attorneys involved in oversight of the psychiatric commitment process. The MDRI team also met with mental health system users and family members. 2
The MDRI fact-finding team conducted site visits at each of two "Colonias" (public psychiatric institutions or asylums located in the countryside), two public psychiatric in-patient facilities in Montevideo, one private psychiatric institution, one institution for boys and adult men with mental retardation and other disabilities, and two community mental health facilities.3 During these visits, team members met with administrators, toured the facility, examined custodial conditions, visited program areas, examined patient charts at random and interviewed system users and staff.
The MDRI team received full access to facilities, patients, and patient records without restrictions. MDRI team members were met with openness and interest by service providers, administrators, representatives of the Ministry of Public Health of Uruguay, members of Uruguay's judiciary, their staff, and all others we interviewed. In addition, representatives of the associations of psychiatric and nursing professions were extremely helpful.
Many of the individuals interviewed by the MDRI team were unsparing in the information and assistance they provided, and they spent a generous amount of their own time with the team, answering questions thoroughly, often with great candor. These individuals provided important insights as to the problems within the mental health system, and they demonstrated a genuine concern for people with mental disabilities. This report would have been impossible without this support.
Three members of the MDRI fact-finding team presented a summary of the report's findngs at a conference organized by IELSUR in Montevideo, Uruguay, August 17 and 18, 1994. Representatives of the Ministry of Public Health, directors and administrators of Uruguay's major public psychiatric institutions, officers of psychiatric and nursing associations, independent service providers, and community leaders (including psychiatric system users and their families) participated in a lively discussion of the report at the conference. Human Rights and Mental Health: Uruguay reflects many of the issues raised at the conference. An advance copy of this report was submitted to the Ministry of Public Health for comment in December 1994. MDRI offered to publish a response by the Ministry of Public Health and offered to wait until March 20, 1995 before going to press. MDRI received no response to our offer.
In individual meetings with government representatives, mental health system administrators, providers, family members, and system users, MDRI team members were encouraged by the widespread support for improving and reforming Uruguay's mental health system. This confluence of interest and concern presents the greatest possible hope for bringing the full protections of human rights law to people with mental disabilities in Uruguay.
This report is not intended to single out Uruguay for criticism but to examine the enforcement of international human rights law that applies to people with mental disabilities universally. The international human rights community should monitor these rights worldwide, and MDRI has begun to do so in South America, Eastern Europe and the United States. The views expressed in this report are those of Mental Disabilities Rights International and the authors and do not represent a position of the Washington College of Law or American University.
I. Introduction
This introduction describes the international human rights standards for the treatment of people with mental disabilities and Uruguay's obligation to reform its mental health system under international human rights law. In addition, the introduction provides background about the historical and political context of Uruguay, including the country's history as an innovator in social welfare programs. Finally, the introduction outlines the organization of Uruguay's present mental health care system.
A. Mental Disability Rights: An International Concern
In the latter half of the twentieth century, there. has been enormous growth in the reach of international human·rights law and its application to people especially vulnerable to abuse. The United Nations has drafted international human rights treaties to protect the rights of women, children, refugees, and ethnic or national minorities. In addition, the United Nations General Assembly has adopted human rights resolutions which set minimum standards in many areas once considered the exclusive concern of domestic policies, including rights in the context of labor and employment, marriage, education, social welfare, the treatment of prisoners, and the treatment of people with mental disabilities.4
The process of establishing international minimum standards for the treatment of people with mental disabilities began in the early 1970's. In 1971, the United Nations adopted the Declaration on the Rights of Mentally Retarded Persons,' and in 1975 the United Nations adopted the Declaration on the Rights of Disabled Persons.6 In the late 1970's and early 1980's, specialized agencies of the United Nations began to develop human rights standards for people with mental illness.
As the United Nations was drafting human rights standards for people with mental illness, regional bodies, such as the Pan American Health Organization (PAHO) took the lead in calling for nations to take concrete steps to assure the protection of human rights for people with mental disabilities.7 In an historic meeting convened by PAHO in November 1990, the Declaration of Caracas was adopted by legislators, non-governmental organizations (NGOs), mental health professionals, and human rights leaders from North and South America.8 The Declaration found that exclusive reliance on the psychiatric hospital "isolates patients from their natural environment ... generating greater social disability. "9 Such conditions "imperil the human and civil rights of patients. "10
The Declaration of Caracas calls on national authorities and NGO's to restructure mental health care systems to "promote alternative service models that are community-based and integrated into social and health care networks. "11 Mental health resources must be used to "safeguard personal dignity and human and civil rights"12 and "national legislation must be redrafted if necessary ... "13 to ensure the protection of human rights.
In December 1991; the United Nations General Assembly adopted the final draft of the Principles for the Protection of Persons with Mental Illness and the Improvement of Mental Health Care (hereinafter the "Ml Principles").14 The MI Principles are the most detailed and comprehensive codification of mental disability rights under international law.15 They provide an instrument for fair and consistent evaluation of human rights practices in mental health systems around the world, applicable across cultures to all levels of economic development. The MI Principles recognize that certain practices will vary from country to country, and according ly, they protect the right of the patient to "treatment suited to his or her cultural background. "16 At the same time, the United Nations working group that developed the MI Principles made clear that the MI Principles are "minimum . . . standards"17 designed to "adequately reflect and accommodate all legal and social systems and all stages of development without sacrificing the essential needs and basic rights of the individual human beings ultimately concerned."18 Thus, the MI Principles state that each country should "implement these Principles through appropriate legislative, judicial, administrative, educational and other measures "19
The Ml Principles apply broadly to people with mental illness, whether or not they are in psychiatric facilities. In addition, the MI Principles apply to "all persons who are admitted to a mental health facility, "20 whether or not they are diagnosed as mentally ill. The Ml Principles protect all such people against discrimination21 and detail a list of rights intended to ensure that people with mental disabilities and other people in mental health facilities are "treated with humanity and respect for the inherent dignity of the human person. "22
The Ml Principtes set out substantive criteria23 and due process protections24 against improper psychiatric commitment. Among the substantive criteria for commitment to a mental health facility, the Ml Principles limit commitment to people diagnosed as mentally ill "in accordance with internationally accepted medical standards."25
The Ml Principles specify that people in mental health treatment have the right to protection against "harm, including unjustified medication . . . "26 "No treatment shall be given to a patient without his or her informed consent ... " (except under special circumstances set out in the Ml Principles).27
The Ml Principles emphasize throughout that "[e]very patient shall have the right to be treated in the least restrictive environment ...."28 Within psychiatric facilities, "[t]he treatment of every patient shall be directed towards preserving and enhancing patient autonomy. "29 In addition, the Ml Principles state that "[e]very patient shall have the right to be treated and cared for, as far as possible, in the community in which he or she lives. "30
Many of the rights in the MI Principles create protections against governmental intrusion upon the lives of people with mental disabilities, while other rights require countries to provide appropriate mental health services.31 Thus, the MI Principles are intended to provide a full range of human rights protections to people with mental disabilities, allowing them the opportunity to enjoy the same freedoms and rights as other people and to live life to its fullest potential.
Since the adoption of the MI Principles, the United Nations has continued to press for the advancement of domestic and international efforts to improve conditions and opportunities for people with mental disabilities. In December, 1993, the General Assembly adopted the Standard Rules on the Equalization of Opportunities for Persons with Disabilities (the "Rules on Equalization").32 In the Rules on Equalization, the United Nations specifies that states should devise policies, 33 develop rehabilitation and other service programs, and reform laws "to create the legal bases for measures to achieve the objectives of full participation and equality for persons with disabilities. "34 To the extent that such programs and legal protections require the investment of resources, "States have the financial responsibility for national programmes and measures to create equal opportunities for persons with disabilities. "35
The Rules on Equalization propose that States "at regular intervals, collect . . . information concerning the living conditions of people with disabilities"36 and create "national coordinating committees, or similar bodies, to serve as a national focal point on disability matters. ,m The Rules on Equalization also call for "international cooperation concerning policies for the equalization of opportunities for people with disabilities."38 Finally, the Rules on Equalization create a Special Rapporteur to monitor implementation of the Rules and to initiate international exchange and cooperation on the improvement of conditions for people with disabilities. 39
B. Uruguay's International Treaty Obligations
The Ml Principles elaborate upon certain protections that are guaranteed by international human rights treaties, to which Uruguay is a party, including the International Covenant on Civil and Political Rights (ICCPR),40 the International Covenant on Economic, Social, and Cultural Rights (ICESCR),41 and the American Convention on Human Rights (American Convention).42 As such, the Ml Principles can be used as a guide to application of human rights treaty provisions to conditions in mental health systems.43. The protections in the Ml Principles relating to civil commitment to a psychiatric institution, for example, protect against "arbitrary detention," as prohibited by the ICCPR44 and the American Convention.45 Practices in mental health facilities which violate the MI Principles and cause great suffering may constitute "inhuman treatment" prohibited by these treaties46 or may violate the right of detained persons to be "treated with humanity and with respect for the inherent dignity of the human person."47
The ICCPR and the American conventions create a legal obligation on State Parties to "respect" and "ensure" the full enforcement of their protections.48 State Parties undertake to take "legislative or other measures as may be necessary to give effect to the rights recognized in the present Covenant. "49 The ICCPR makes no exception to the duty of full enforcement for rights that may require the investment of resources, and rights may be limited ("derogated") only "[i]n time of public emergency which threatens the life of the nation and the existence of which is officially proclaimed. "50
Uruguay is also urrder an obligation to ensure the "highest attainable standard of physical and mental health" under the ICESCR.51 Countries can work toward this treaty obligation by establishing mental health policies consistent with the minimum standards established by the MI Principles. For example, policies consistent with the principle that "the treatment of every patient shall be directed toward preserving and enhancing patient autonomy"52 or the principle that "[e]very patient shall have the right to be treated and cared for, as far as possible, in the community ... "53 can be considered a step toward the enforcement of the treaty obligation to ensure the highest attainable standard of mental health.
Unlike ICCPR, which creates an immediate duty of full enforcement, the ICESCR creates a duty of "progressive enforcement." No country can produce the "highest attainable" standard of mental health overnight, but each Party to the ICESCR "undertakes to take steps ... to the maximum of its available resources, with a view to achieving progressively the full realization of the rights" established under the Covenant.54 Even though outcomes may only be achieved over time, "the obligation 'to take steps' is an immediate one .... At minimum, this might involve the drawing up of a detailed plan of action for the progressive enforcement of the right. "55 The steps taken should be "deliberate, concrete and targeted" to the full enforcement of rights.56
The ICESCR's requirement that a State take steps "to the maximum of its available resources" does not specify which of its national resources can be considered "available" for reform.57 At minimum, State Parties to the ICESCR must use resources currently available in mental health budgets to enforce policies that will uphold the rights established in the ICESCR. Even where resources are limited, the obligation to "devise strategies and programmes" for the promotion of rights established in the ICESCR "are not in any way eliminated as a result of resource constraints. "58
As this report demonstrates, improper treatment practices in Uruguay's mental health system raise fundamental human rights concerns. Yet the identification of human rights violations is not meant to suggest that the individuals working within Uruguay's mental health system intend to cause danger or suffering.59 On the contrary, MORI encountered a large number of staff dedicated to the well-being of people in their care. The reforms proposed in this reort are necessary so that same staff dedication can be properly re-directed toward treatment that is appropriately respectful of the rights of people with mental disabilities.
C. Political & Historical Context of Uruguay
Uruguay is a small country of approximately three million people located on the Atlantic coast of South America between Argentina and Brazil. Uruguay's per capita gross domestic product is the forty-fifth largest in the world (on approximately the same level as Hungary and Greece), but it is ranked twenty-ninth according to the "Human Development Index" of the United Nations Development Program (UNDP).60 The UNDP ranking reflects the fact that Uruguay has a high rate of literacy,61 an excellent system of higher education,62 a long life expectancy, and many good social welfare programs. Although social programs have been cut back in recent years, the distribution of income in Uruguay is still the most egalitarian in Latin America.63
1. Welfare state, dictatorship and democracy
From the late nineteenth century to the mid-twentieth century, Uruguay enjoyed a long period of economic growth and political stability. During this time, Uruguay developed some of the best and most innovative social welfare programs in the region. A period of economic decline began in the 1950's and continued into the 1960's. In 1973 the military took power.
The military held power for twelve years in what was a brutally repressive regime.64 After a 1980 plebiscite in which the military government was surprised by a vote against a constitution that would have legitimized its power, the military allowed general elections. On March 1, 1985 the military government stepped down and the winner of the election, Julio Marfa Sanguinetti of the Colorado party, was allowed to take office.
2. Impact of economic decline and dictatorship
Uruguay's formidable array of public benefits began to decline in the 1960's as the economy faltered, and social programs were further cut back during the dictatorship. Hospital administrators and representatives of the Ministry of Public Health reported to MORI that the dictatorship caused a period of stagnation in the mental health system when major reforms were impossible. When the military came to power in 1973, the worldwide move toward treatment of people with mental disabilities in the community had just begun to influence thinking about mental health service planning in Uruguay. After the coup, innovation became difficult or impossible. The result was the maintenance of the status quo - reliance on large, custodial hospitals for the treatment of most people with mental disabilities. Few, if any, community alternatives to large psychiatric hospitals were developed in the 1970's and 1980s.
3. National Program for Mental Health
Shortly after the re-establishment of democracy, there were efforts to restore and improve social programs that had been allowed to languish during the dictatorship.65 The Ministry of Public Health initiated a new effort to study and plan comprehensive reform of the mental health system. 66 The Ministry of Public Health established an inter-disciplinary commission of thirty six representatives of all sectors of the mental health system (the "National Commission") , which produced a program for national reform, the Programa Nacional de Salud Mental (the "National Program"). 67 The National Program proposed two main goals for reform: (1) the development of a community-based mental health system integrated within the general health care system and (2) the establishment of a campaign on prevention and rehabilitation. The plan emphasized the importance of an inter-disciplinary approach to mental health treatment in which families would be integrally involved in prevention and rehabilitation. When it was completed in 1986, the National Program was approved by the Ministry of Public Health, and its goals are the official policy of the Ministry today.
Psychiatrists, social workers, and nurses interviewed by MDRI reported that, following the adoption of the National Program in 1986, there was a widespread feeling of hope that major changes would take place in the mental health system as a result of the National Program. As of 1993 when the MDRI team visited Uruguay, however, the National Program had not been implemented. Neither the National Commission nor the Ministry of Public Health ever calculated the cost of implementation,68 and the legislature never appropriated the necessary funds. Despite this, Ministry of Health Officials report that some elements of the National Program have been put into effect. As recommended in the National Program, there was a move toward the decentralization of mental health services, with mental health units having been established in public hospitals outside of Montevideo. A mental health unit was established in Maciel Hospital in Montevideo to be the first receiving hospital before patients were transferred to other hospitals. In addition, the Ministry of Health and administrators at the Colonias engaged in significant efforts to address life-threatening conditions at the Colonias, such as insufficient food and heat.
In recent years, as Uruguay's economy stagnated, the Ministry of Public Health has been subject to budget cutbacks, leaving the mental health system even further from the goals set forth in the National Program for reform.69
D. Organization of Uruguay's Mental Health System
There are both private and public mental health services in Uruguay. Sixty percent of the population receives health care (including access to mental health care) through "mutualistas,"70 networks of private hospitals and physicians that provide services under governmentally mandated insurance plans. Most working people in Uruguay are required to become a member of a mutualista. Thirty percent of the population who have not paid to be part of the mutualista system may receive services through the public health care system. Additional private services also exist, serving wealthier individuals and government employees.71
1. Mutualistas
Limited outpatient and inpatient mental health care is available through mutualista hospitals, consisting almost entirely of pharmacological treatment. No patient management, vocational programming, rehabilitation, or psychotherapy is available through mutualistas.
Outpatient care is provided by psychiatrists at mutualista hospitals and "policlinicas" (outpatient clinics). Outpatient care consists of very brief visits with psychiatrists (usually 10-15 minutes) for the purpose of prescribing medications and monitoring blood levels of medications. The mutualista will pay for the cost of inpatient care at a private, mental health facility for up to thirty days. Such facilities often do not provide any psychiatric treatment programs themselves, so mutualista psychiatrists will visit patients in these facilities to oversee the prescription of psychotropic medications and the administration of ECT. Private inpatient mental health facilities do not exist outside the capital, Montevideo. Thus, all private inpatient care outside Montevideo is provided through mutualista general hospitals.
2. Public hospitals
The public mental health care system services individuals who have no other form of insurance and cannot provide for their own private care. It also provides for long-term patients who have used up benefits provided through the mutualista system.
The public mental health system consists almost entirely of inpatient facilities, with some treatment to outpatients. There are just over 2,000 inpatient psychiatric beds in the country (.06% of the three million people in Uruguay).72 According to the Ministry of Public Health, the cost of care to the government is twenty to twenty-five dollars per day for each inpatient psychiatric bed.
Public inpatient beds in Uruguay are divided between two "Colonias" (Santin Carlos Rossi and Etchepare) located ninety kilometers outside of Montevideo, housing a total population of just above 1,300, and two psychiatric institutions in Montevideo, Musto and Vilardebo, with populations of 600 to 650, respectively.
According to Ministry of Public Health officials, the average length of stay in the Colonias is at least ten years. At Musto and Vilardebo, the Ministry of Public Health reports that the average length of stay is approximately one year. The MDRI team was not able to verify these figures, but there is evidence to suggest that the average length of stay at each of these institutions may be much longer.73
There are no public, inpatient services for the treatment of alcohol or substance abuse.
Protective shelters for people who are homeless are not available.
3. Disability pensions
A pension system for people unable to work due to mental disabilities is available through the social security system. Only individuals who have worked and paid into a social security system are eligible for this pension, equivalent to eighty to one hundred dollars per month.
To qualify for disability, individuals must demonstrate that they .are unable to work. Thus, if a person on disability gets any form of paid work, he or she loses disability payments entirely (regardless of whether the individual's total earning are sufficient to live on). Recipients of disability benefits, family members, and social workers complained that this rule is a disincentive to find jobs. Since the pension is not enough to live on, patients living in the community are reported to work "off the books." This practice makes it difficult to find jobs and results in individuals working without any legal protections or benefits.
4. Professional resources
Uruguay is rich in human resources and has a well educated population. The country has a plentiful supply of psychiatrists and psychologists, but there is a great shortage of professionals with more basic and widely applicable skills - such as psychiatric nurses and psychiatric social workers.
There are more than 450 psychiatrists registered with the Uruguay Psychiatric Association,74 a relatively high concentration of psychiatrists per capita by world standards.75 Most psychiatrists are trained in the country at the University of Uruguay medical school. There are approximately 2,500 psychologists in Uruguay with a five-year college degree.76 Most psychologists are psychoanalytically trained and take patients in private practice.
There are a large number of trained psychiatrists and psychologists currently working in private practice in Uruguay who could potentially contribute an enormous amount to the mental health system. There are also many low-paid mental health professionals and non-professionals who could contribute much more than they now do, but who can only afford to work part of the time in the public mental health system. Within each institution, MDRI found a core of the staff who demonstrate great commitment to their work and to the well-being, dignity, and rights of patients. These individuals, many of whom work at other jobs, work very long hours on behalf of patients in public facilities.
There is a great potential for new opportunities for mental health professionals to contribute to the improvement of services. More and better mental health professionals could be attracted to working in the public sphere, and individuals now working in the public mental health system might contribute more as they saw their efforts come to fruition.
There is a great shortage of other professionally trained staff. Because of low pay in the public mental health system, public hospitals are generally not able to hire sufficient numbers of specialized nurses and social workers.
According to representatives of the Association of Nurses of Uruguay, there are 1,800 university trained nurses in Uruguay, but very few work in public psychiatric institutions because of the low pay. There is reported to be a great shortage of trained psychiatric social workers in the country, and only a few work in public psychiatric facilities.77 The great majority of staff, known as "tecnicos," are non-professionals with only in-service training.
5. Services for victims of human rights abuses
The Servicio de Rehabilitacion Social (SERSOC) is a non-governmental organization established to provide mental health care to individuals and families suffering from the post traumatic effects of torture, disappearances, and other abuses under the dictatorship. Psychologists, social workers, psychiatrists and other physicians volunteering their time and working at low pay for this organization have helped more than 3,000 clients. SERSOC estimates that they have been able to serve only a small portion of the population who have experienced severe mental health problems as a direct or indirect result of abuse. Despite this, the organization receives no support from the public or private mental health care systems.
II. Human Rights Conditions
The primary findings of MDRI's investigation of human rights conditions in Uruguay's public mental health system are described below. Section A describes the structure of Uruguay's mental health system and the human rights implications of a system based almost exclusively on in-patient treatment. Section B describes Uruguay's civil commitment law, its implementation, and analyzes the extent to which it comports with international standards. Section C describes conditions in Uruguay's psychiatric facilities and identifies practices that violate international human rights standards,78 and Section D analyzes the extent to which oversight mechanisms exist to ensure the enforcement of international human rights in the mental health system.
A. Structure of Public Services
Medical and human rights standards adopted by the Pan American Health Organization (PAHO) in the Declaration of Caracas and the United Nations General Assembly in the Ml Principles call for governments to structure service systems to ensure support for people with mental disabilities in the community.79 As the Ml Principles provide, "[e]very person with a mental illness shall have the right to live and work, as far as possible, in the community. "80 In addition, every patient has the right "to be treated in the least restrictive environment. "81
One of the most noticeable aspects of Uruguay's mental health system is that it relies almost entirely on psychiatric institutions. This near-exclusive reliance on institution-based treatment results in the unjustified, unnecessary, and potentially harmful institutionalization of people capable of safely living and working in the community.
The segregation of patients in hospitals often breaks down personal, family, and economic ties to the outside world and results in a decline in social and mental health functioning. The Ministry of Public Health, psychiatrists, nurses and others noted their concern to MDRI with regard to the imbalance of services, and they have attempted to remedy this situation. There are a number of impressive community mental health programs in Uruguay.82 These programs provide essential services that allow a small number of individuals to leave institutions and receive mental health care in the community. Such programs serve as an Uruguayan model for mental health services which allow people to receive support and treatment in their own communities.
1. Custodial institutionalization
Uruguay's mental health institutions have two functions, acute care and long-term care. Long-term patients receive essentially custodial care, which includes psychotropic medication and a limited number of in-hospital activity programs. Staff at the Colonias informed MORI that the primary emphasis of care is on maintaining individuals within institutions rather than providing rehabilitation and returning individuals as quickly as possible to the community from which they have come.
The lack of emphasis or urgency placed on rehabilitation and reintegration into the community can be seen·throughout Uruguay's public mental health facilities. The problem of custodial institutionalization is particularly extreme for at least half of the 2,000 individuals in the public system who are labelled "chronic patients" and are thought to have little or no potential for return to the community. Indeed, "chronic patients" live ten, twenty, thirty years or their whole lives in the psychiatric facility. Many "chronic patients" receive no rehabilitation programming that might give them the hope of ever leaving the institution. Most residents of the Colonias are reported to live there until they die.
Custodial hospitalization adversely affects other patients who only need acute care. Overcrowding makes it difficult to find beds for some acute patients. By stretching the already inadequate rehabilitation and out-placement services at institutions (described in Section C below), "short term" stays in the institution last for unnecessarily long periods of time. At Musto, a facility designed as an acute care facility, the average length of stay is reported to be one year (the average length of stay at Musto may well be much longer, however, given the large number of long-term patients).
2. "Social patients"
Authorities at Uruguay's public psychiatric institutions reported to MORI that between one-third and two-thirds of the 2,000 inpatients have no need to be committed to a psychiatric institution but are held there because they have no place else to go. These individuals are commonly known as "social patients." According to institution authorities, all of these individuals could be moved out of institutions if appropriate community facilities were available.
Officials and mental health system administrators expressed great concern about "social patients," and they observed that the dislocation of these individuals stems from problems that go far beyond the mental health system. Indeed, the mental health system is forced to cope with the effects of a range of social problems - including poverty, unemployment, the lack of affordable housing, and the breakdown of family support systems - that are not necessarily linked to mental health. These social problems cannot be solved alone by Ministry of Public Health officials or institution administrators.
The ranks of the social patients include four categories of individuals:
(1) People who may once have needed hospitalization
The first category of social patients are individuals with mental illness who may once have required psychiatric hospitalization but who could now live safely in the community with appropriate community treatment. This includes "short-term" or "acute" patients, who are likely to leave the institution eventually, as well as "chronic" patients who may only leave the institution after many years. For both populations, the unnecessary length of their stay increases the difficulty of returning to the community as family and economic ties to the community are weakened and lost.
At Colonia Rossi and Colonia Etchepare, there is a particularly large number of long term "chronic" patients who have lost almost all contact with the outside world. Many of these individuals are elderly and neither need nor receive any form of psychiatric treatment but may require nursing care.
(2) People with other disabilities or illnesses and elders
The second category of social patients may have no mental illness but have another disability or illness for which they may require community support, such as mental retardation, epilepsy, or alcoholism. In the Colonias, one-third to one-half or more of all residents may have mental retardation.83 All these individuals could function in the community,84 but specialized services suited to their needs are lacking. Psychiatric institutionalization is particularly inappropriate for people with mental retardation, because these individuals are particularly vulnerable to abuse and neglect. In Uruguay's psychiatric institutions, no habilitation services are provided to meet their special needs; instead, they often receive psychotropic medications or ECT that may be inappropriate to their needs.
In institutions, MORI also found elders who lack family or who are unable to take care of themselves. MORI documented the case of an elderly woman who lived by herself with many cats and other pets. When neighbors complained to the police about the sounds and smells of the pets, the woman was placed in a psychiatric hospital. Upon arrival at the institution, psychiatrists determined that the woman was not mentally ill, but she was held there because no other placement could be found for her. Unlike many other social patients, this woman was eventually able to leave the institution because a placement was identified for her in a nursing home.
(3) Petty criminals, social outcasts
A portion of social patients without mental illness are detained in institutions by judicial order. Among the people in this category are petty criminals who may also be alcoholic or mildly mentally retarded, or may simply display bizarre behavior of one form or another that leads judges to refer them to psychiatric institutions rather than to prisons. As a result of this disposition, however, the individual will be subject to an indefinite period of detention, possibly longer than if convicted of the petty crime for which he or she may have been charged. Mental health officials are unable to release these individuals without a judicial order. This problem is discussed further in section B-4, below.
In one case, MDRI team members interviewed a patient who was reported to be a lesbian. Although thi patient was also mildly mentally retarded and could have been hospitalized as a "social patient" on that ground alone, the fact that she was a lesbian apparently contributed to the difficulty of returning her to the community. Indeed, the director of one institution said that gay and lesbian patients were excluded from one outpatient placement program for fear of antagonizing people in the community.
(4) People who are homeless
A fourth category of institution residents have no mental illness, and may have no other disability, but are homeless or have no other place to go. At Vilardebo Hospital, we interviewed a Brazilian woman who was living in the institution while waiting for official papers to be approved and for financial assistance from her family to come so that she could return home. A sixteen year-old woman at Colonia Etchepare reported to us that she lived in the Colonia because she was born to two patients in the institution.
The institutionalization of people who are homeless is a graphic illustration of the mental health system being assigned a responsibility that has nothing to do with mental health. The government of Uruguay must take responsibility for this problem, which cannot be solved by officials of the mental health system alone.
3. Lack of community-based alternatives
The Ml Principles provide that "[e]very patient shall have the right to be treated and cared for, as far as possible, in the community in which he or she lives. "85 Many people are forced to stay in institutions because there is a great shortage of community-based alternatives. In addition to the 1,400 or so individuals considered to be "social patients" in public hospitals, there is almost certainly a need for community services for individuals in private psychiatric facilities and among individuals currently receiving no mental health treatment. In addition, many other current residents of public psychiatric facilities not labelled "social patients" by the institutions might well prosper in the community if services were available.
The Substitute Family Program, which places former residents of the Colonias with families, is a very impressive model. The program provides payments to families who are willing to take in a former psychiatric patient. Although payments to families are small (the equivalent of approximately thirty-eight dollars per month) there is no shortage of families willing to take in psychiatric patients. The program not only provides a home in the community for former long-term residents of the Colonias, it provides follow-up services that protect the safety and promote the well-being of the former patient, including mental health care and assistance in finding a job. The program also builds upon existing community structures, making contacts for the patient with churches, civic associations, and social welfare programs.
Although organizers report that the substitute family program needs additional funds, it now functions on strikingly small government contributions. The program could be greatly expanded without large increases in funding.
There are also both governmental and non-governmental models for supportive mental health services in the community. The public mental health system currently supports one rehabilitation program in the community, the National Center for Psychiatric Rehabilitation. The National Center provides a setting for psychiatric treatment and rehabilitation of forty to sixty people with mental disabilities, as well as a supported work program for eighty participants. Each program participant is evaluated by an inter-disciplinary team of psychiatrists, psycholo gists, and social workers, and an individual treatment plan is developed. Mental health treatment is discussed with the patient, and no coercive treatment is provided. Participants in the rehabilitation program live on their own or with families and come to the rehabilitation center for a half or full day of crafts, recreation, and occupational therapy.
The National Center for Psychiatric Rehabilitation is the only community facility in the public mental health system. In addition, four or five private community mental health treatment centers also exist. MDRI visited one such facility, the Sur Palermo Rehabilitation Center, which provides structured programs for the rehabilitation of sixteen to twenty former psychiatric patients in a supportive environment. Staff and service users are considered "members" of a co equal community, and no treatment is provided without the user's understanding and consent. Former members and their families reported to MDRI that the Sur Palermo program provides an effective service that helps former psychiatric patients live in the community and avoid re hospitalization.
The two community mental health programs reviewed in this report demonstrate that Uruguay has the technical resources and know-how to develop community facilities, and can do so with a limited infusion of public resources. In addition, they demonstrate the cultural relevance and practical value of programs built on respect for the choice and rights of system users.
In addition to the lack of mental health services in the community, there is also a lack of many other kinds of services that would allow people to leave psychiatric institutions. There is a particularly great need for habilitation and support services for people with mental retardation. Almost every person with mental retardation now living in an institution could function in the community with a great improvement in quality of life.86 Despite this, the MDRI team was not able to locate a single supported living program in Uruguay that would allow adults with mental retardation to function in the community. There are also reported to have been recent cutbacks affecting community programs for people with alcoholism and for homeless shelters.
Finally, the resources available to increase community-based alternatives to institutions that do exist have not been fully tapped. In addition to serving as models for new programs, existing community mental health programs could be expanded with only small increases in government support. The Director of the National Center for Psychiatric Rehabilitation explained that his facility is currently operating under capacity. Without an increase in staff or office facilities, the Center could take another ten or twenty patients. The staff of the substitute family program also explained that there are more families willing to take psychiatric patients at the current rate (approximately thirty-eight dollars per month per patient) than there are currently funds to support. The Sur Palermo and SERSOC programs receive no governmental funding at all.
B. Civil Commitment
Civil commitment to psychiatric institutions in Uruguay is regulated by the law of "Assistance to Psychopaths."87 The law, first enacted in 1936, fails to provide the minimum protections against improper commitment set out in the MI Principles with regard to both substantive criteria and procedural protections. 88 In practice, not even the minimal require ments of Uruguay's commitment law are enforced.
1. Lack of criteria for commitment
Article 15 of the law of Assistance to Psychopaths provides generally that involuntary commitment by medical order is authorized only for "treatment purposes."89 While the law limits involuntary commitments to patients certified as "mentally ill," there is no further definition of what constitutes "mental illness." No other substantive criteria are required for most involuntary commitments.9°
The commitment law of Uruguay fails to contain the MI Principles' minimum substantive standards that would limit involuntary commitment to individuals who are dangerous to themselves or others,91 or to individuals who, because of severe mental illness, require treatment that cannot be provided outside the setting of a psychiatric hospital.92 In addition to its failure to define "mental illness," the law does not require that a determination of mental illness "shall be made in accordance with internationally accepted medical standards. "93
Despite its weaknesses, the commitment law of Uruguay might prevent the hospitalization of half the patients now in Uruguay's public psychiatric institutions if the law were actually enforced. As described in section A-2 above, authorities estimate that one-third to one-half of the population of the Colonias are placed in the institution because of mental retardation and not mental illness. A range of individuals now hospitalized because of epilepsy, alcoholism, old age, or petty criminal behavior would be excluded from institutions by law if they are not mentally ill. "Social patients," who by official accounts constitute approximately half the total patient population, are hospitalized because "they have no place to go" and not for the purpose of psychiatric treatment as required by Uruguay's commitment law. Thus, full enforcement of Uruguay's commitment law would require and end to the practice of detaining "social patients."
2. Lack of procedural protections
Commitment procedures under the law of Assistance to Psychopaths fail to provide protections against improper commitment both as a matter of law and as a matter of practice.
a. Commitments under Uruguay law
Under Uruguay's law, individuals may be subject to involuntary commitment in four ways, by (1) medical certification,94 (2) emergency medical commitment,95 (3) emergency police commitment,96 or (4) judicial order.97 According to institution authorities, the great majority of patients are admitted by medical certification, and only ten to fifteen percent are admitted by judicial order.98 Only one to two percent of patients are reported to be admitted to the institution as voluntary patients.
Three of the four methods of commitment (except judicial commitment, which is described further in section C-4, below) entail a certification process which may include approval by the institution medical director, independent physicians, family or police (these three methods of commitment are described here as "commitment by certification"). In all three forms of commitment by certification, the admitting physician must notify an "Inspector General of Psychopaths"99 and a judge within twenty-four hours. Neither the Inspector nor the judge are required to act on this notification.
Since there are no substantive criteria for determining who can be committed in most cases (except "mental illness" and "for the purpose of psychiatric treatment"), the certification process under the law of Uruguay requires only the consent of the person providing certification. There are no limits on the discretion of the individual providing consent.
"Medical certification," the most common way individuals are committed to psychiatric institutions (and the procedure with the fewest protections), requires consent of the receiving physician at the hospital, and two physicians who must agree that the individual is "mentally ill." In addition, there must be consent by the patient's closest relative, legal representative, or an adult living with the patient. Since medical certification is always an option, any additional protections created by other forms of commitment can be circumvented
Not surprisingly, the three methods of commitment by certification in the 1936 mental health law of Uruguay do not provide the procedural protections contemplated by the MI Principles. Although a court must be "notified" within twenty-four hours of any involuntary commitment, 100 there is no right to a review of commitment by a "judicial or other indepen dent or impartial body."101 None of the methods of commitment by certification provide an individual subject to involuntary commitment with a right to "appeal to a higher court." 102 Nor does the individual have the right to counsel,103 or to "attend, participate, or be heard personally in any hearing. "104
The Ml Principles do not provide relatives or legal representatives with the right to commit a psychiatric patient, and international law generally does not allow one person to waive another individual's rights. In lieu of rights provided to the person subject to commitment, however, the rights that Uruguayan law delegates to family members could provide protections against some improper commitments. Even so, not even this minimal protection is consistently enforced. Many family members reported to MDRI that they were never asked permission when their relative was committed. Some family members who were asked to consent said that they considered it a formality - they were provided with no information about the commitment and they never believed they actually had a choice.
One mother reported being able to prevent commitment by refusing to consent, but she said that this proved to be a difficult experience. When she refused, psychiatrists tried to go around her by asking other members of the family to authorize commitment. According to the mother, the institution psychiatrist told other relatives that her judgment was impaired due to stress and exhaustion. Despite this, none of the other relatives agreed to provide authorization, and the commitment did not go forward.
b. Inspector General of Psychopaths
One of the potentially most important protections under the law of Assistance to Psychopaths, is an office called the "Inspector General of Psychopaths" (lnspecci6n General De Psic6patas).105 The Inspector is intended to provide independent oversight of the commitment process and to monitor the enforcement of the mental health laws generally.106
The admitting physician at a psychiatric institution must notify the Inspector within twenty four hours of any commitment and must provide a certificate explaining the patient's symptoms and conditions. 107 The Inspector may help family members who seek release of a relative from a psychiatric institution by bringing a case to the attention of judicial authori ties.108 The Inspector must keep a general registry of everyone civilly committed.109 In order to monitor the enforcement of mental health laws, the Inspector may conduct unannounced visits to psychiatric institutions, send warnings to institutions about improper commitments, or notify courts of potentially criminal wrongdoing.110
Despite these intended protections, the practical value of this law has been limited. From the early 1970's until 1992, the position of Inspector of Psychopaths was vacant.111 In October 1992, one month before the visit by the MDRI team, the position was filled for the first time. The new Inspector, serving as an independent ombudsman, could potentially provide important protections to patients subject to civil commitment. Yet the current law establishes significant limitations on the Inspector.
The most important limitation on the value of the Inspector is that patients do not have a right to review of commitment by the Inspector, nor do they have a right to participate in the review in any way. The investigation of any particular case is now entirely up to the Inspector's discretion. This limitation is particularly serious, given the lack of a right to a hearing by an independent review body under the commitment law. The power of the Inspector is also limited by the weakness of the underlying commitment law that the Inspector is empowered to enforce.
The new inspector has an enormous task before him to make up for the years of improper commitments. 112 The Inspector reported to MORI that his first major project would be to modernize and computerize the psychiatric register, which contains information about every person who has ever been committed to a psychiatric hospital.113 In addition, the Inspector said that he planned to institute a new system to require institutions to obtain informed consent of families before providing ECT.
The Inspector stated that, within a year, he intends to review every psychiatric commitment in the country of more than sixty days, beginning with commitments at private psychiatric facilities. The Inspector's method for a review of commitment, which he demonstrated while a member of the MORI team was in his office, is to telephone the director of a psychiatric institution and ask about the well-being of a particular patient. If the director states that the patients is present and still mentally ill, the review is complete. While this method of review may help up-date the psychiatric register, it provides almost no human rights protections to the patient: The current method provides no opportunity to review whether an individual meets substantive criteria for commitment, it provides patients with no due process protections or opportunity to present their views or concerns, it provides no independent check on the authority of psychiatric institutions, and it provides the Inspector with no independent information about the conditions and possible abuse of psychiatric patients.
The Inspector acknowledges also that there is a problem of patient access to his services. After two months in office, very few, if any, patients were aware of his office, and no patient had yet contacted him with a problem. In response to this situation, the Inspector also stated that he would insist that all private psychiatric institutions provide patients with access to tele phones. The Inspector told MORI that any private institution that does not provide patients with access to a telephone would have its license revoked within a few months.
3. Indefinite length of commitment
The Law of Assistance to Psychopaths provides only indefinite commitment and places no practical limitations on the discretion of medical authorities to retain a person in an institution. Most patients may be discharged only when the treating physician determines that there is no more need for treatment. 114
The law further provides that individuals who have at any time been subject to "restraint of liberty" within an institution can only be released when "they are no longer dangerous. "115 The law does not provide a right to discharge, however, to a patient who is no longer dangerous.
The Uruguay law requires that an attending physician provide reports to the Inspector General of Psychopaths when a patient is involuntarily committed, transferred, released, or when a patient escapes.116 The MI Principles provide patients with a right to a full, periodic review of commitment by a review body (a "judicial or other independent or impartial body") at intervals established by law.117 Patients involuntarily committed by medical certification have no such right under Uruguay's commitment law.
4. Additional problems of judicial commitment
The fourth method of commitment is by judicial order. A person may be committed by judicial order if a judge finds him or her incompetent to stand trial or if a judge determines, for any reason, that an individual should be committed.118
People subject to judicial commitment face a number of special problems. Uruguayan law requires judicial approval before they can be released.119 There are no applicable laws or standards in Uruguay for guiding the decision to release a person from the institution. According to the President of Uruguay's Supreme Court, the decision is left entirely to the discretion of the judge. Some judges are reported to obtain an independent psychiatric assessment of the patient before ruling on the case.120 Occasionally, judges are reported to order individuals to remain in the institution even though both the institution and an independent psychiatrist determine that a patient is no longer mentally ill or dangerous. Judges are not required to issue a written order or explain their reasons for keeping an individual in the psychiatric hospital.
Until recently, according to institution administrators, judicially committed people with no need for hospitalization could spend years in the psychiatric institution without having their case reviewed by a judge. There was no periodic review of commitment and no mechanism for bringing the case to the' attention of the judge. In 1991, the Supreme Court of Uruguay authorized the Judicial Information Service, an office made up of two attorneys, to take responsibility for identifying individuals ready for discharge and bringing such cases to the attention of a judge.
Despite the creation of the Judicial Information Service, institution directors and staff complained of cases in which patients with no need for hospitalization would wait weeks or months for judicial discharge. The MORI team interviewed three individuals who had received medical discharges but were awaiting judicial approval for their release. The staff of the Judicial Information Service agreed that there is a backlog of cases, and they explained that they are overwhelmed by the number of cases they must review.121
At some institutions, such as Vilardebo, everyone who is judicially committed is placed on the security ward.122 Thus, the effect of judicially commitment can be harsh, because conditions on the security ward are generally worse than in other parts of the hospital. Conditions are particularly poor on the security ward at Colonia Etchepare, and they are worse than other parts of the institution at both Vilardebo and Musto (see discussion in Section C, below). At Colonia Etchepare and at Musto, the authorities reportedly move individuals in and out of the security ward at their own discretion, but at Vilardebo, authorities report that they cannot do so without approval by a judge.123
5. Conditional discharge
The Law of Assistance to Psychopaths has a special provision for "conditional discharge" that allows the director of an institution to retain control over a patient even after he or she leaves the institution and order his or her return at any time.124 Conditional discharge is legally not to exceed three months except in a "special case" which may continue for up to two years (a "special case" is not defined). In practice, people (including participants in the "substitute family" program, described below) are reported to be formally or informally kept on conditional discharge indefinitely.
Even if the upper time limit were enforced, there are a number of problems with conditional discharge under the law of Uruguay. There is no limitation on who may be subject to conditional release. Thus, even the most highly functioning individual with no trace of mental illness can be kept on conditional discharge. Once a person is on conditional discharge, there are no medical or behavioral standards for which a patient can strive in order to be fully released from the mental health system. Patients on conditional release may be recommitted at any time at the discretion of the director without any of the formalities required under the commitment law of Uruguay.
C. Conditions in Institutions
The Ml Principles include the right of people in institutions to protection against harm and unjustified medication, 125 the right to "be treated with humanity and respect for the inherent dignity of the human person,"126 and the right to treatment "directed towards preserving and enhancing personal autonomy. "127 Treatment and conditions that unnecessarily prolong hospitalization violate the right to treatment in the least restrictive environment.128
Human rights conditions in Uruguay's public in-patient psychiatric facilities are described below. The MORI team visited Colonia Rossi and Colonia Etchepare, large public facilities located ninety kilometers outside Montevideo that housed 716 and 670 people, respectively, at the time of the MORI visit in November 1993. Within Montevideo, the MORI team visited the two other public psychiatric facilities, Musto and Vilardebo, which had a November 1993 census of 373 and 260, respectively.
In all the public institutions visited by MORI, the team found problems that administra tors are struggling to address. These include old buildings with poor physical conditions, inadequate staffing, certain improper treatment practices characteristic of custodial institutions, and a general lack of protection of patients' rights and dignity. Independently and together, these deficiencies render it more difficult to rehabilitate and reintegrate patients into the community. Unnecessarily long hospitalization and lack of case management leads to the loss of social, family, and economic ties to the community. Psychiatric hospitalization in Uruguay creates unnecessary health risks and contributes to a decrease in social functioning and psychological well-being.
1. Poor physical conditions
The Ml Principles require conditions in institutions to be "as close as possible to those of normal life" to include respect for the patient's dignity, privacy, recreational and leisure activities, education, and vocational rehabilitation.129 Since the end of the dictatorship, the Ministry of Public Health has undertaken initiatives to address what were once life-threatening conditions, including inadequate food and heat and necessities like blankets and mattresses. This initiative has resulted in important improvements in physical conditions.
Physical conditions in the Colonias are reported to be much improved over the way they were five or six years ago. Some buildings have been cleaned and modernized, and plumbing has been fixed, and the basic hygiene of Colonia residents is improved. In Vilardebo, the MDRI team observed similar physical improvements, such as new electrical wmng. MDRI also observed impressive new facilities for outpatient services at Vilardebo.
Despite improvements in recent years, the physical facilities at all four public psychiatric facilities are nevertheless not "as close as possible to those of normal life," as required by the MI Principles. They are impersonal, lacking in privacy, and almost completely barren of decorations or conveniences of daily living. The Colonias, located on green campuses in the countryside, have the potential for being beautiful settings for rehabilitation, exercise, or other activities, but few activities appear to be available.130 Although some of the buildings at the Colonias are new or modernized, many are old and decrepit. A few areas smelled of urine and feces at the time of the MDRI visit, and there were flies in many of the buildings. Vilardebo, built in 1880, is now run-down and crumbling, its gardens neglected and overgrown. Although staff were mopping and cleaning in parts of Colonia Rossi and Vilardebo at the time of the MDRI visits, the tile floors were so old and stained that they appeared dingy even after they were cleaned. Musto is the most modern of the four public facilities, yet its atmosphere is also dreary and impersonal.
a. Poor environment for rehabilitation
Most patients in Uruguay's public psychiatric facilities live in large wards of twenty, thirty, or more patients with beds in long rows and little other furniture. There is generally no decoration, no usable space for personal possessions to be kept, and no place where residents can go to be alone. Generally, each patient's bed is the only space or object that is even slightly private. There are almost no personal effects and no reading material on the ward. We saw few clocks or calendars on the ward to mark the passing of time.
In some of the institutions, the residential wards lack day rooms for recreation or other activities, or even any comfortable place to sit. At Colonia Rossi, patients must sit in benches in the dining area in order to watch television. In the most modern hospital, Musto Psychiatric Hospital, there is one room on each ward intended to serve as a day room and a dining room. In most cases, this room was almost completely barren of decoration or furniture at the time of the MDRI visit. We observed patients at Musto eating standing up or leaning against a window sill.
b. Unhygienic conditions
Basic sanitation is a problem in the security wards of each hospital. In the Musto security ward, walls and floors were covered with graffiti and dirt, windows were unclean, and the bathroom was flooded at the time of the MDRI visit. In the locked ward at Colonia Rossi, some patients were wandering about naked, and there was a smell of feces. In an isolation room, there was a filthy sponge mattress on the floor.
At the Colonia Etchepare Security ward, the worst area reviewed by the MDRI team, toilets and sinks were clogged, and water from the toilets was on the floor in the hallway and sleeping area. Many beds were broken or without mattresses, and some patients were sleeping on the bare floor. There are no facilities for heating food, and meals brought in from the kitchen are reported to be regularly served cold. Late in the summer there is reported to be a shortage of water in the Colonias that makes cleaning more difficult and less frequent.
2. Inadequate number of professional staff
The MI Principles state that mental health systems must provide "[q]ualified medical and other appropriate professional staff in sufficient numbers ... to provide each patient with. . . a program for appropriate and active therapy."131 Lack of staff may also result in improper treatment and unjustified use of medications, violating the MI Principles' right to protection against harm.132
Facilities in Uruguay have many people on staff, but there is a shortage of trained and adequately compensated professionals. Although there are, technically, adequate numbers of psychiatrists, their availability to patients is limited due to economic conditions that force most psychiatrists to work more than one job. Psychiatrists are generally unavailable for extended contact with patients or adequate monitoring of the effects of medications. There are severe shortages of psychologists, nurses and social workers throughout the public mental health system, in large measure due to low pay. In practice, most care is provided by non-professional tecnicos.
a. Low salary, absenteeism
Low salaries and poor working conditions at psychiatric institutions result in high levels of absenteeism and a generally poor quality of professional service. The salary for psychiatrists ranges from $450/month for the director of a psychiatric institution to as low as $200 or $150/month for other physicians and psychiatrists. As a result, medical staff take one, two, or more additional jobs. A number of psychiatrists confided to the MDRI visitors that they were often too exhausted by overwork and dispirited by conditions in the institution to give their best work to their job for the public facility.
Salaries for some social workers, nurses, and non-professionals in public facilities are even lower. Social workers and nurses receive as little as $100/month. At Musto Hospital, the absenteeism rate is reported to be as high as fifty to sixty percent.133
There is reported to be a problem of low morale among many of the staff who show up to work. These staff members, who also work more than one job, report working very long hours and being overwhelmed by the tasks that need to be done at the public institutions. Despite these problems, the MDRI team observed a small core of individuals at each institution who appear very devoted to their work.
b. Shortage of specialized professionals
Although Uruguay has many psychologists, the vast majority of these individuals work only in private practice. There is also a great shortage of psychiatric nurses and psychiatric social workers in Uruguay, leaving the work in psychiatric institutions to nurses and social workers without any specialized training in the needs of psychiatric patients. Many other specialists are completely lacking, particularly professionals trained to provide habilitation or other programming to people with mental retardation. Despite the large numbers of people with mental retardation in public institutions, the MDRI team did not find a single social worker or psychologist trained to provide services to this population in any of the public facilities, the Colonias, Vilardebo, or Musto.
Nurses and social workers are not hired in sufficient numbers to serve institution residents adequately. At Colonia Rossi, there are two psychologists, three occupational therapists, two nurses, and eight social workers for a total patient population of 716. In addition to working outside the Colonias, some of these professionals never see patients because their work is purely administrative. In Musto hospital, six social workers serve 373 inpatients and approximately 700 outpatients. Since these social workers all work extra jobs, they go off duty at two every afternoon.
The shortage of professional staff undermines the effectiveness of the ones who come to work and are devoted to the care of patients. The social work staff at Musto, for example, is responsible for helping patients obtain daily services within the hospital, maintaining contacts outside the hospital, and assisting patients with discharge planning. Since the social work staff is so overwhelmed by the number of patients it serves, many patients must wait months to receive assistance with discharge planning. As a result, institutionalization is prolonged, contacts with family, friends and employers break down, and discharge planning becomes much more difficult.
Institutions not adequately staffed with psychologists, social workers, and other professionals are not able to provide patients with rehabilitation, case management, and other activities necessary to allow patients to build and retain social or vocational skills and to return to the community when ready. Most of the time, patients are left to the care of untrained tecnicos. Authorities at Musto, one of the better staffed institutions, reported that during the day there are often no mental health professionals available on the ward. During such times, there is often one tecnico on duty for every 100 patients in the institutions.
c. Custodial care
With such staffing limitations, the psychiatric institutions of Uruguay can provide little treatment. The activities of the tecnicos observed by the MORI team were limited - cleaning up after patients or standing in nursing stations waiting for the occasional emergency. The tecnicos explained to the MORI visitors that they provide medications, keep patients out of fights, and occasionally restrain patients who become unruly. The tecnicos lack the training, direction or leadership from higher level staff to enable them to take a more active role with patients. During MORI visits, team members observed very little interaction or conversation between staff and patients. As a result, most patients were left to complete inactivity most of the day - wandering the haHs of institutions, sitting by themselves or in groups, or lying in bed.
In the various institutions visited by the MORI team during daylight hours, between ten and sixty percent of psychiatric patients were in bed at any given time. Among patients who were awake, there was a striking lack of meaningful activities.
The failure to provide structured activities in institutions is compounded by rules and regulations that inhibit patient initiative at all levels. At Musto Hospital, for example, a woman hospitalized for epilepsy described her feelings after three months in the hospital:
I would like to go out. They are not letting me go out, even to the park. I feel suffocated. Sometimes I want to die because I feel so bored.
While some patients explained that they are allowed outside the building, complaints about constant and unending boredom represented the most common concern that the MORI team heard from psychiatric patients.
3. Treatment practices
The MI Principles include the right to appropriate health care,134 and mental health treatment "directed towards preserving and enhancing personal autonomy. ,ms People in psychiatric treatment also violates the right to be "protected from harm, including unjustified medications. "136
As in many custodial institutions, treatment in Uruguay's psychiatric facilities is almost entirely limited to somatic therapies (psychotropic medications and electroconvulsive therapy ("ECT")). The proper use of these treatments is limited by inadequate treatment records and the lack of documented diagnoses. In addition, opportunities for the return of many patients to the community are limited by the lack of support for rehabilitation.
a. Treatment records
One necessary component of adequate treatment is a complete treatment record. The MI Principles require such records, including documentation of all treatment137 and a full treatment plan.138 Records must also indicate whether treatment is voluntary or involun tary.139 MORI was only able to review a few patient records a each facility, but none of the records reviewed by the MORI team included a full treatment plan or an indication of whether treatment was voluntary or involuntary.
Treatment records in Uruguay's psychiatric institutions are generally very spare and without narrative. For- the most part, they record the date, time, and dosage of medications prescribed, without explanations for levels of medication or changes. The records often do not specify a complete diagnosis, nor do they provide more than a very limited social or medical history of the patient. The records showed scant evidence of physical examination and generally little or no evidence of medical information integrated into the psychiatric assessment. No individualized treatment plans or progress notes (including essential information about patient responses to medications) were observed in any of the major public psychiatric institutions. Based on these records, coupled with the minimal use of laboratory work and the lack of other instruments for assessment (described in subsection c below), it is impossible to assess whether a psychiatrist properly prescribed psychotropic medications. Without adequate records, treating psychiatrists cannot consistently evaluate the effects of any particular treatment.
In the one private hospital MORI visited, record keeping practices were similar to those in public institutions. By contrast, at the National Center for Psychiatric Rehabilitation, medical records contained full narrative histories, individualized treatment plans, progress notes, and discharge plans. These records explained how the individuals responded to the program of therapy and why each change in the program was made.
b. Diagnosis
The MI Principles require that a determination of mental illness be "in accordance with internationally accepted standards. "140 Proper diagnosis is essential to provide care to a patient "appropriate to his or her health needs," as required by the MI Principles.141
Even where psychiatrists reported that internationally recognized diagnostic systems are used,142 MDRI observed little or no reference to specific diagnoses in medical records. In general, diagnoses are no more specific than "psychotic," or "schizophrenic." Often, the only additional detail in the record is whether the patient is viewed as "acute" or "chronic. "
MDRI reviewed a number of records of individuals with no psychiatric diagnosis. One chart stated that a patient was admitted for a "behavioral disorder." Other charts provided no indication of the reason for hospitalization. Institution authorities explained that large portions of the institution population have no psychiatric diagnosis on their record because they are not mentally ill. Among those who lack a psychiatric diagnosis are one-third to one-half of the population of the Colonias who are reported to be mentally retarded,143 as are a substantial portion of the patients at Musto and Vilardebo.
c. Psychotropic medication
The Ml Principles require that "every patient shall be protected from harm, including unjustified medication. "144 Neuroleptic medications can be effective in controlling symptoms of certain medical disorders and are used throughout the world. It is generally accepted that they must be used and monitored carefully, however, because they have serious side effects.145
In certain cases, they can slow or inhibit a patient's capacity to return to the community.146 They can also cause great suffering,147 permanent debilitation from tardive dyskinesia,148 and even death from neuroleptic malignant syndrome.149 In Uruguay, the Ministry of Public Health has established an approval process for psychotropic medications and a formulary for approved medications.
The lack of specific diagnosis and complete medical records on the ward renders it difficult or impossible to determine whether psychotropic medications are safely and effectively used in public psychiatric institutions. Based upon the review of a small sample of records at public psychiatric institutions and reports by psychiatrists at these institutions, however, there are a number of other potential problems that warrant further investigation and review, including: inadequate monitoring of each patient's medical history and side effects, unnecessarily high dosages of psychotropic medication, and polypharmacy .150
Standard medical practice includes taking social and medical history into account as well as monitoring for adverse side effects of psychotropic medications ."1 The patient records reviewed by the MORI team were not sufficiently detailed to permit physicians to note all relevant history or fully monitor side effects to adjust medication levels accordingly. Records reviewed showed a lack of information about monitoring for side effects regarding particular bodily organs, such as bone marrow (through complete blood counts), thyroid, liver, and kidney (though laboratory profiles). Records also demonstrated a lack of documented physical assessments, such as the AIMS (Abnormal Involuntary Movement Scale) to assess for tardive dyskinesia, an often irreversible and potentially debilitating involuntary movement disorder. Many records lacked evidence of adequate monitoring of blood serum levels of medications (e.g. lithium, valproic acid, and carbamazepine) which can be toxic at certain levels.
A number of the medical records reviewed revealed a practice of polypharmacy. Polypharmacy, the simultaneous use of multiple medications of the same class or with the same intended therapeutic effect, can be dangerous for the patient. 152 Drugs of the same class have cumulative effects, increasing the risk of side effects and adverse reactions to the drugs. Since polypharmacy makes it almost impossible to determine the exact impact of each medication prescribed, it renders proper monitoring of side effects more difficult. It also makes it difficult to identify which medications are particularly effective in controlling symptoms of mental illness.
Polypharmacy may be warranted in a particular case for special reasons. In such cases, though, it is important to document the reasons in the chart so that outside reviewers can evaluate the appropriateness of the prescription.
The MDRI team reviewed records in which two, three, four or more psychotropic medications were simultaneously prescribed for a particular patient. One sixty-nine year old woman with a diagnosis of "melancholia" was listed as concurrently receiving the following medications: Notropil, Haldol, Chlropromazine, Lorazepan, Bromazine, Imipramine, Paranox (staff reported this to be a hypnotic), as well as arthritis drugs and Piportil.153 The records of another patient with a diagnosis of "chronic psychosis" stated that he was on Haldol, Tegretol, and Neuroleptil simultaneously.154 Upon first admission, the same patient had been ordered to receive Chlorpromazine, Levopromazine, Taractin, and Chlorpretexeno.155
Two records of patients with mental retardation reviewed by the MDRI team reveal that each patient was prescribed multiple neuroleptic with no medical justification in the chart. In one case, a woman with mental retardation and no other psychiatric diagnosis was prescribed the neuroleptics Neuroleptil, Chlorpromazine, and Taractan. Another woman with mental retardation was prescribed carbamazepine (Tegretol) 20-30 mg, Haloperidol, Diazepam, and Profenamia (Parsidol) 150 mg/day.156 The medical record also stated that "if she gets excited, inject Nozinan and Fernergan intra-muscular."157
Staff recognized the importance of monitoring blood levels for certain medications, but they were impeded in their ability to engage in this work. Progress notes and laboratory reports showed that blood levels of lithium and Tegretol are not closely monitored. At Musto, a psychiatrist explained that there was a slow process for getting lab results back for patients on Valproic acid, Tegretol, or Lithium, which hinders monitoring potentially toxic levels of these medications.
As described below, no procedures are in place to allow for informed consent to psychotropic medications, as the MI Principles require.158 Although many patients were aware of the name and dosage of medications they had been prescribed, no patient interviewed by MORI reported that he or she had been given any information about potentially negative side effects. In general, institution authorities reported that patients are not given any role in the decision about whether to take a particular medication. According to a staff member at Colonia Etchepare, one reason for this is that because psychiatrists consider it to be potentially harmful for the patient to be so informed. Sometimes families are consulted about medication.
MDRI is also concerned about dosage levels of neuroleptic medications, which appeared to be relatively high. The effect of high doses of many psychotropic medications is to sedate patients.159 This may impede a patient's participation in rehabilitative activities in the hospital and preparation for a return to the community.160 Although MDRI did not review a sufficient number of records to make findings on dosage levels, two facts require further inquiry. First, an official at Musto said that many patients do not participate in activities because they are on high dosages of medication. Second, large numbers of patients in Uruguay's institutions appear heavily sedated, lying in bed or shuffling from place to place without engaging in any meaningful activity.
d. Electroconvulsive Therapy (ECT)
Electroconvulsive therapy (ECT) is a recognized treatment for severe depression, but it is a potentially dangerous treatment that can cause short-term memory loss.161 Thus, ECT should be restricted to uses in which its efficacy has been clearly demonstrated (e.g. severe depression).162 As with. other forms of treatment, the Ml Principles require that ECT be limited to patients for whom it is "appropriate to his or her health needs"163 and does not cause unjustified "harm ... mental distress or physical discomfort."164
The frequency of ECT use and the modality of treatment varies by institution.165 According to institution authorities at Colonia Rossi, Colonia Etchepare, and Musto, ECT is frequently used to control "aggressive behavior" in patients who may or may not have any psychiatric diagnosis. Records reflected this use. At Musto, where institution authorities report that 10% of the patient population receives ECT at any one time, ECT is reported to be used for a wide variety of conditions, including aggressive behavior by people with mental retardation.
MDRI reviewed the records of two patients at Musto with mental retardation who had received extensive ECT, even though they had no psychiatric diagnosis. In one case, a twenty seven year old woman with mental retardation and no psychiatric diagnosis received ECT once a week for almost a year. There was no explanation in the record as to what the ECT was supposed to accomplish. The limited narrative in the record states only that she "is aggressive, she constantly escapes from home, she walks and screams." There is no indication that behavioral therapies were used or attempted. The record states that she had several previous admissions at Vilardebo Hospital, and she appears to have been kept continuously at Musto for the last two years.
Authorities reported that bilateral ECT is generally used, a practice which is no more effective than unilateral ECT and which has greater risks of memory loss. The ECT inspected by MDRI are older "sine wave" machines rather than "brief pulse. "166
Patients are not asked for their consent to take ECT (see discussion in section B-5). Where institutions seek consent, they ask families, not patients, for approval. Information on ECT's negative side effects is not provided.
e. Rehabilitation and psychotherapy
In addition to requiring that treatment be directed towards the enhancement of personal autonomy, 167 the Ml Principles specify that institutions must provide "appropriate vocational rehabilitation measures to promote reintegration in the community. "168 Not only is rehabilita tion limited in Uruguay's public mental health facilities, but the environment permits long-term inactivity, leading to the loss of social or occupational skills that patients may have had when
. they entered the psychiatric hospital.
Some rehabilitation programs exist at each psychiatric hospital, and MDRI observed a few rooms equipped for rehabilitation activities. At Musto and Vilardebo, the rehabilitation programs described by institution administrators closed down for three months during the summer, leaving no activities for patients. Even when these programs are in operation, however, they serve only a small proportion of patients in the institution. During MDRI's visits to four public psychiatric facilities, the vast majority of patients were not engaged in any meaningful activities. During the course of our visit, MDRI observed no more than a handful of patients actively involved in a rehabilitation program.
The most extensive workshop is run by the National University of Labor at Colonia Etchepare, which provides classes in sculpture, woodworking, and furniture repair. MDRI received very positive reports by patients who participated in a theater program at Colonia Etchepare. At Musto the MDRI team observed a carpentry shop. None of these programs were in operation at the time of the MDRI visit in late November because summer vacation had already begun.
In addition to the pervasive lack of planned activities, there are few opportunities for patients to engage in constructive activities on their own initiative. At the Musto and Vilardebo institutions, there is almost no place for such activities. At Musto, there is a barren room called a "day room" in which there is little or no furniture. In the wards at Colonia Rossi, the only place to sit is in the dining rooms. There is a special building set aside for activities, however.
f. Internal mechanisms for quality assurance
The MI Principles require the establishment of "appropriate mechanisms ... to promote compliance with these Principles. "169 -The MDRI team found no evidence of internal controls for quality assurance regarding psychiatric treatment, no incident or utilization review, and no evidence of chart review or of ongoing assurance for the quality of medical records. There is reportedly no internal mechanism for accident or incident reporting.170 Given the lack of proper staffing, medical records, and monitoring of the effects of psychotropic medications, the lack of internal controls presents special dangers for psychiatric patients. The Ministry of Health expressed interest in establishing quality assurance programs, and MDRI encourages them to do so.
There is a lack of continuing education for professional staff at institutions. According to reports by institution psychiatrists, staff training in the use of psychotropic medication comes largely from pharmaceutical companies.171 The institutions have contracts with the companies for medication, and the company provides training sessions in the use of the medication under contract. There appears to be no education at all on behavior training for people with mental retardation.
4. Patient choice and patient rights
There is little or no recognition that patients in psychiatric institutions have legal rights. Upon commitment to a psychiatric institution, the authorities control almost all aspects of the patients' lives, large and small. Psychiatric commitment itself is almost entirely left to the discretion of psychiatrists and administrators, as described above. Every other aspect of the patient's life in the institution - what kind of medication a patient receives, when a patient eats, sleeps, goes outdoors, or uses the telephone - appears to be subject to the discretion of institution authorities.
Among some staff, there is a recognition that patients have "rights," but the expression of these rights is subject to the discretion of institution staff. For example, one psychiatrist explained that while "patients have a right to refuse [treatment], the doctor has the right to override the patient's decision." Another member of the professional staff at Musto said to MORI, "the psychiatric hospital is the legal protector of the patient."
a. Recognition and notice of rights
The concept of patients' rights is known and recognized in Uruguay. In 1992, the Parlia ment of Uruguay adopted a Patients' Bill of Rights,172 incorporating various rights from the American Association of Hospitals, the Council of Europe, and the Hospitals of Catalufia, Spain. Among the many provisions of the Bill of Rights, is the recognition that every patient has the right to be informed of his or her rights as a patient, to be treated respectfully, to refuse to be examined or observed by any particular care giver, to have a treatment plan, and to receive complete information about diagnosis, treatment, and prognosis. Every patient has the right to "participate in decisions affecting treatment," and the right to report complaints about treatment without being subjected to punishment.
Like the Patients' Bill of Rights of Uruguay, the MI Principles require that patients in psychiatric facilities be given effective notice of rights.173 MDRI found almost no notice of rights within public psychiatric facilities. On the door to the chief social worker's office at Musto, there was a short list of patients' rights, and in the same office, there was a poster regarding the Judicial Information Service. In our entire tour of psychiatric facilities, however, the MORI team observed no other listings of patients' rights, nor did we observe any written sign of formalized complaint procedures.
b. Informed consent to treatment
The Ml Principles provide patients with a right to informed consent to treatment174 and a right to refuse treatment.175 The right to refuse treatment under the Ml Principles is not absolute, but the right can only be limited by an independent authority or by mental health practitioners under limited circumstances and through procedures set forth in the Ml Principles.i1,
Professional staff at Colonia Etchepare and Musto report that psychiatrists generally do not provide information to patients about the effects of medication. Moreover, there is no system for establishing informed consent. A member of the professional staff at Colonia Etchepare reported that there is a common understanding that it is not a good idea to tell patients about their treatment. In part, the staff member explained, this information could contribute to a patient's problems. In·addition, the staff member said that it would present an enormous logistical problem to inform patients of the effects and side effects of medication. ("There are so many patients that they could not possibly do it"). Despite the general practice of not informing patients, some psychiatrists are reportedly careful to inform patients about the effects of medications.
Six of fourteen patients interviewed by a member of the MDRI team at the Colonia Etchepare, Musto, and Vilardebo institutions were able to name medications that they had received. None of the patients interviewed by MDRI said they had been informed about potentially negative side effects of medications.
Non-professional tecnicos at the Colonia Etchepare security ward reported that they have standing orders to provide psychotropic medication by injection to patients who refuse medication or who become aggressive or unruly. Consent is not required, and approval of a physician or psychiatrist is only required if such treatment is to continue for longer than a day or two.
According to the Inspector General of Psychopaths, psychiatrists are required to seek judicial approval to order ECT against the will of a psychiatric patient. According to three patients interviewed by MDRI, however, consent to ECT was never an issue. In each case, a psychiatrist ordered ECT and the patient received it without ever being asked for consent or being informed about side effects.
c. Family consent
The MI Principles do not allow consent to treatment or to the waiver of any of an individual's rights by members of his or her family. A "personal representative" for a person who lacks capacity for a certain decision may only be appointed after a hearing by an "independent and impartial tribunal," at which a patient has a right to counsel.177
The Inspector General of Psychopaths reported that no procedure currently exists for obtaining the informed consent of patients or family members to psychotropic medication or ECT. He said that he is planning to institute a new procedure for establishing the informed consent of family members to ECT. In the future, the Inspector says that he will institute a similar form for consent to psychotropic medication. The Inspector mentioned no intention to introduce procedures to obtain patients' informed consent to treatment.
Current practice regarding family consent appears to be varied. Some family members in Uruguay report that they are occasionally asked to provide consent to ECT on behalf of their relatives. Two of nine families MORI interviewed said that public psychiatric institutions asked for authorization to administer ECT, while other relatives reported that they were never asked. Similarly, the majority of families reported that they were never informed about the side effects of ECT. A number of family members explained that private psychiatric institutions regularly ask for permission to perform ECT because the family must agree to pay for the treatment.
In one case, members of a family reported objecting strenuously when a psychiatrist ordered a series of eight administrations of ECT for their son. ECT was administered on one occasion despite their objections, but the series was discontinued.
d. Reproductive rights/parental rights
Institution staff report that there has long been a problem of children being born in the Colonias because of the lack of birth control. At the Colonias, patients are rarely provided with birth control. According to institution staff, a psychiatrist or physician may prescribe birth control pills or order a woman to be fitted with an IUD if she "appears to have many lovers." In fifteen years of working at Colonia Etchepare, however, one staff member reported being aware of only ten to twelve patients who received any form of birth control.
When a woman gets pregnant and gives birth in a psychiatric institution, and there is no family outside the institution prepared to take the baby, the baby is taken away from the mother after four or five days and given to !NAME, Uruguay's governmental adoption agency. !NAME will place the baby with a foster family, and the mother will have up to one year to regain her child. To regain the child during the one year period, the mother must first be released from the institution and ruled mentally competent. If the baby is not claimed during this time, all birth records are destroyed, and permanent foster parents are assigned. Any future contact between mother and child becomes impossible.
Institution staff report that, even though mothers have a right to regain custody of their child for up to one year after it is taken away, women who may qualify to regain custody often cannot do so because they- are not informed about the procedures for regaining custody. Thus, mothers who are committed to a psychiatric institution for a short period of time often permanently lose parental rights over their children.
The systematic failure to involve the child's natural parents in the decision to place a child in foster care or to inform them of their parental rights violates international human rights standards, 178 as does the lack of opportunity for parents to the return of their child.179
D. Oversight
International human rights treaties to which Uruguay is a party require the state to ensure the safety and well-being of people in psychiatric facilities.180 The MI Principles specify that "[s]tates shall ensure that appropriate mechanisms are in force to promote compliance with these principles."181 The MI Principles require regular inspection of facilities "with sufficient frequency to ensure that the conditions, treatment and care of patients comply with these Principles. "182 The MI Principles require generally that "[e]very patient shall be protected from harm, including unjustified medication, abuse by other patients, staff or others or other acts causing mental distress or physical discomfort. "183
There is no independent oversight of conditions or treatment in Uruguay's mental health system. Nor are there effective mechanisms to promote compliance with the MI Principles.
1. No standards for quality control
Psychiatric facilities operate entirely without quality controls. This is a serious problem, given the broad range of treatment practices in Uruguay's psychiatric institutions that can have dangerous side effects.184 Administrators at two hospitals expressed eagerness to have some standards for assessing quality of care, at least for their own internal guidance and evaluation.
Institution administrators at three major public institutions report that the Ministry of Public Health regularly monitors the use of government funds but makes no effort to regulate the quality of services at institutions. Indeed, institution administrators report that there are no standards for assessing the quality of services that institutions provide.185
One official explained that the Ministry of Public Health does not regulate quality of care in institutions because every institution is supposed to have its own ethics committee to supervise quality of life and treatment practices. At the same time, ethics committees are widely understood to be non-functional, and in some institutions they never meet. In any event, ethics committees are no substitute for quality assurance mechanisms.
The Director of the Mental Health Section of the Ministry of Public Health stated that his office is currently supervising the creation of various task forces to establish treatment standards in a number of areas, including the use of ECT, psychotropic medications, and sterilization. He informed MORI that the first task force report would be completed in 1994. He said the report would set standards for the use of ECT and would rely heavily upon standards set by the American Psychiatric Association. One of the Ministry's goals in setting standards is to reduce the number cases in which ECT is administered on patients whose conditions do not justify its use.
The Director of the Mental Health Section pointed out that his work is limited because the Ministry of Public Health does not have legal authority to establish binding standards. For standards to be binding, the legislature would have to enact a new law providing the Ministry of Public Health with authority to set such standards.
2. Inadequate regulation of service providers
Although the Ml Principles require competent authorities to assure "[q]ualified medical and other appropriate professional staff,"186 there are only very limited mechanisms for monitoring the qualifications of service providers. Psychiatrists are licensed, but there is no public or independent system for setting or monitoring standards of psychiatric care. One psychiatrist is reported to have lost his license to practice after he was criminally convicted of misusing narcotics. There is no system for licensing psychologists or other mental health professionals.
3. No procedures for reporting or investigating unusual incidents
To ensure enforcement of the Ml Principles, procedures must be available for the "submission, investigation and resolution of complaints. "187 MDRI found no mechanisms in place at any of the public psychiatric institutions for reporting patient concerns, improper treatment practices, medication errors, misuse of seclusion or restraints, violence against patients, sexual assault, unnatural deaths, or any other unusual incidents. Staff at Colonia Etchepare and Musto report that patients with problems regularly come to social workers, and the social work staff will help to the extent that they can.
Institution staff and attorneys at the Judicial Information Service reported that there are no formalized complaint procedures, 188 no independent system of investigation, and no established remedies for abuses in institutions."9 Unless they have resources to hire a private attorney, patients do not have access to counsel.190
While institution administrators at each institution denied that dangerous treatment practices or violence on the ward was a problem, MDRI team members collected a number of reports to the contrary. At Colonia Etchepare, staff reported that there is an extensive problem of sexual assault and potentially abusive sexual relations. Sexual relations among patients or between patients and staff are reported to take place frequently, and the institution has no guidelines to determine when such practices are proper and when they are not. No procedures exist to investigate relationships that are potentially abusive. On rare occasions the institution does investigate allegations of abuse, but this is reported to be limited to situations in which a member of the staff takes up the cause of a particular patient and brings attention to the matter.
III. Hope for Reform: Strengths of Uruguay's Mental Health System
Despite the serious nature of the human rights concerns surrounding Uruguay's public mental health system as well as the limited resources available for reform, Uruguay has the potential for tremendous progress. The greatest strengths of Uruguay's mental health system lie in the human resources available and the widespread concern about the problems within the system. There are also a number of impressive mental health programs in the community that serve as useful models for reform.
MORI was encouraged to find widespread interest in improved mental health care and human rights enforcement on the part of Ministry of Public Health officials, service providers, and advocates. Representatives of psychiatric and nursing professional associations expressed an interest and a willingness to take risks necessary to bring about mental health system reform. In addition, the MORI tea:m met with an organization of families and mental health system users aware of the problems in the mental health system and committed to working to bring about reform. The establishment of a broad coalition of interested community members, including human rights advocates, such as IELSUR, can be invaluable in building public support for reform. Leadership on the part of interested non-governmental organizations will be essential to provide the sustained attention necessary to transform public support into action for reform.
Many of the human rights concerns raised by MORI in this report were identified in 1986 by the National Mental Health Commission. The ambitious national reform plan, the National Program for Mental Health, would restructure services to create a primarily community-based mental health system. Although the legislature of Uruguay has not allocated the funds necessary to implement the National Program, the plan still represents official policy and a positive set of aspirations for reform on the part of the Ministry of Public Health. Although the National Program needs revisions since it was produced six years ago, it can serve as a blue-print for reform.
Since the development of the National Program, the United Nations has adopted the MI Principles. The MI Principles provide both guiding concepts and specific examples that can be used to update and direct a new program for the National Program. This report is intended to demonstrate the major changes needed in the mental health system to bring it into conformity with the MI Principles. The newly adopted United Nations Rules on Equalization provide guidance to the Government of Uruguay about how meet its obligations to reform by initiating a national planning process that includes consultation with non-governmental organizations and the full participation of people with mental disabilities.
The Ministry of Public Health can provide leadership in bringing Uruguay's mental health system into conformity with international human rights standards. By adopting the progressive National Program as its official policy, the Ministry of Public Health has already made an important statement about the need for change. Now that the United Nations has adopted the Rules on Equalization, the Ministry of Public Health should act immediately upon its commitment to reform by developing a plan for implementing the National Program and this report's recommendations.
The power to address all the concerns raised in this report goes beyond the domain of the Ministry of Public Health. The large number of social patients, the absence of services in the community for people with mental retardation, and the problems with the 1936 mental health law, for example, cannot be solved by the Ministry of Public Health alone. Other relevant branches of government must also take action, and Uruguayans must work together to enable people with mental disabilities to live with dignity and with respect for human rights.
IV. Recommendations
Under international human rights law, governments bear the responsibility of human rights enforcement. The government of Uruguay should take the following actions to bring Uruguay's mental health system into conformity with international human rights law:
A. Structure of Services
A-1 End the detention of "social patients" - The practice of using psychiatric hospitals for the commitment of people with no bona fide diagnosis of mental illness or people with no current need for psychiatric treatment should be terminated immediately. In particular, long-term hospitalization of persons who are mentally retarded or alcoholic is inappropriate.
A-2 Conduct system-wide review of commitments - The government should establish a process for evaluating current residents of mental hospitals, especially for the Colonias, to determine if there is a present need for inpatient psychiatric care and to resettle in the community all patients who are not in need of inpatient psychiatric hospitalization.
A-3 Create community-based alternatives - There is an urgent need to develop community mental health programs to provide for the residential, clinical, and psychoso cial rehabilitation and vocational/employment needs of persons who are mentally ill. Such services are needed both by patients who are currently hospitalized unnecessarily, and to prevent resorting to unnecessary hospitalization of other mentally ill individuals in the community.
A-4 Create services for people with mental retardation in the community - The lack of any community alternatives for people with mental retardation, and the terrible mistreatment of such people in institutions is in part a product of the lack of knowledge of the enormous strides in the habilitation and community integration of people with mental retardation. Training in skills to serve people with mental retardation can be the first step toward the creation of a comprehensive system for habilitation.
In the field, the concept of "habilitation" or training has become central, since mental retardation is not an illness or a disease. Psychologists (not psychiatrists or other physicians) have developed ways of training people with mental retardation to increase their skills in many ways, including skills in daily living (dressing, grooming, cooking, eating, toileting), getting around independently (taking the bus), and, for many, working. Experts in the field should be brought to Uruguay so that parents and professionals can be trained and the basis laid for improving the lives of people with mental retardation. The training should cover all facets of habilitation, including activities of daily living, behavioral training, independent living, and vocational training.
A-5 End disincentives to work in pension benefits - By cutting off benefits to people with disabilities who earn less than subsistence income, the social security law creates disincentives to work. The law should be amended to encourage work on the part of people with disabilities.
A-6 Include psychiatric coverage in mainstream health care - The severe limitations on psychiatric coverage in mainstream health care need to be addressed so that psychiatrists are given options for their patients other than medication and hospitalization. Psychotherapy and other mental health services should be covered.
With or without a further legislative mandate, Uruguay's Ministry of Public Health should:
A-7 Take a leadership role in restructuring the mental health system - The Ministry of Public Health can and should exercise leadership in bringing about reform of Uruguay's mental health system. While some changes are beyond the Ministry's control, it can take action immediately on the following:
- a. Showcase community-based models - Uruguay now has a number of impressive models for reform, including the National Center for Psychiatric Rehabilitation, the Substitute Family Program, and private community mental health programs, such as the Sur Palermo Community Mental Health Center. The Ministry of Public Health can support and draw on these models as it presses for the creation of nation-wide community mental health programs.
- b. Bring in outside reviewers for comprehensive monitoring - This report raises
only a few of the major human rights concerns of people within the mental health system of Uruguay. A major, thorough and well-documented review of conditions in mental health facilities would be a very helpful tool in pressing for system-wide reform. Outside reviewers should be brought in to examine conditions. These reviewers should have enough time to examine charts to assess medication practices and ECT administration. - c. Arrange trainings - Training in many of the skills necessary for the creation of community mental health programs are now lacking. The Ministry of Public Health can play an instrumental role in bringing in experts to train professionals in occupational therapy and psychiatric rehabilitation.
- d. Establish standards of care - The Ministry of Public Health should establish standards of care on its own initiative for institutions and community programs. These standards can then be used to monitor and evaluate programs.
- e. Seek legislative reforms - Even without additional funds, the Ministry of Public Health can take a leadership role in developing policies leading toward reform. As part of its commitment to creating a community-based system of mental health care, the Ministry can seek legislative reforms (such reforms, to include amending Uruguay's civil commitment laws and establishing effective quality control and oversight mechanisms, are outlined in recommendations C and D below). The Ministry of Public Health can use the process of legal reform and quality control to familiarize the legislature and the public with the MI Principles and with the human rights concerns of people in mental health facilities. By involving a broad base of Ministry of Public Health officials, concerned professionals, system users, family members, and advocates in the development of institutional standards, a coalition for reform will open up the day-to-day life of people in institutions to public scrutiny.
A-8 Involve system users in reform efforts - Current and former users of the mental health system should be actively involved in the process of restructuring the mental health system. Not only do users have a right to have their concerns heard, but in addition their experience in identifying the deficiencies of the current system will be invaluable.
A-9 Publicly present a plan for implementing reforms, including a budget and a timetable, to the legislature - The Ministry of Public Health should evaluate the cost of implementing the National Program for Mental Health as well as this report's recommendations to bring the mental health system in line with the MI Principles. Uruguay may need to invest additional resources to restructure its mental health system, particularly to create community-based mental health services, and the implementation plan should include a realistic estimate of these new costs. The Ministry of Public Health's plan should estimate both the cost of creating services in the community and the savings that will arise from closing institutions. Finally, the plan should include a realistic timetable with concrete objectives for action.
B. Civil Commitment
B-1 Revise mental health law - The mental health law is in urgent need of revision in light of developments in international law governing civil liberties and human rights. In particular, a reformed mental health law should:
- a. Adopt substantive standards for commitment consistent with the MI Principles. Civil commitment should be limited to individuals with a bona fide diagnosis of mental illness and clear and convincing evidence of being endangered or dangerous to others by reason of mental illness
- b. Adopt procedural protections consistent with the MI Principles. These provisions should include the right to a review of commitment by a judicial or other independent body, a right to appeal commitment to a court, a right to counsel in commitment proceedings, and a right to present evidence
- c. Provide for periodic review of commitment at regular intervals set by law. The law should also be changed so that hospitals can release involuntary patients who no longer need psychiatric treatment without obtaining a judicial order
- d. Ensure the enforcement of rights in institutions. Oversight mechanisms should be built into the law so that rights in institutions are fully enforced (See D-1, 2, and 3 below).
- f. Ensure methods for reporting and investigating abuses. The law should establish a system for reporting patient complaints and allegations of abuse. An independent system for investigating such allegations should also be instituted.
C. Conditions in Institutions
C-1 Adopt treatment standards - There is an urgent need to adopt a set of professional standards governing the operation of psychiatric hospitals. There are many available models for such internationally accepted standards which the government could review prior to adopting. These standards should address all aspects of the operation of psychiatric hospitals, including:
- a. admission and discharge practices
- b. individual evaluation and treatment planning
- c. restrictions on patient Iiberties
- d. protection from harm
- e. general living conditions for patients in psychiatric hospitals
- f. clinical indications for the use of psychotropic medications and electro-convulsive therapy
- g. guidelines for prescribing medications including polypharmacy and co-pharmacy
h. regular and periodic evaluation of patients for the presence of side effects of medications
Standards for the use of medications should include:
- i. a prescription policy
- J. prescription procedures
- k. a pharmacy manual
- I. specific controlled substances information
- m. psychotropic drug treatment regimen
- n. protocol for patients on medications
C-2 Ensure broad-based involvement in development of standards - In addition to ensuring that important diverse perspectives will be represented, the development of standards for institutions can be a way of raising awareness of the issues and deficiencies within psychiatric hospitals.
C-3. Refer to practice guidelines - As an adjunct to standards, psychiatrists in many countries use practice guidelines. These guidelines should be made widely available to psychiatrists in Uruguay. A list of suggested guidelines is attached in the bibliography.
C-4 Use internationally accepted diagnoses - Services providers should follow the International Classification of Diseases 10 (ICD(lO)) or the recently released Diagnostic and Statistical Manual of Mental Disorders IV (DSM IV) as the agreed-upon classifications for diagnostic purposes. These should be reflected in medical records.
C-5 Build treatment upon community supports - In addition to the treatment standards listed in B-1, the treatment of the individual should be seen within the social context of the family, the community, and a network of caring providers and support groups.
C-6 Conduct a thorough review of medication and ECT practices - A thorough, independent review of medication and ECT practices should be undertaken in the Colonias and other public and private hospitals according to internationally accepted standards, under the auspices of the Pan-American Health Organization (PAHO) or other similar organization.
C-7 Investigate pharmaceutical marketing/research practices - In conjnnction with the medication review, the nature of pharmaceutical marketing and research practices should be explored to determine whether reforms are necessary.
C-8 Improve treatment plans/records - The process of maintaining and keeping records should be dramatically improved, so that records reflect internationally accepted practices as to diagnoses, nursing observations, medication reviews and other critical aspects of a chart. The right to an individual treatment plan has now been recognized under the MI Principles, and this right should be fully ensured.
C-9 Establish quality assurance system - Quality assurance must be an integral part of the service-delivery system. Utilization review and a special review manual from the United States and other countries are available, and similar systems should be adopted.
C-10 Establish continuing education requirements - Mental health professionals should all be required to enroll in regular continuing education classes in the areas of their expertise. The government should ensure that classes are available so that international advances in treatment can be incorporated into practice in Uruguay.
C-11 Problems of staff morale should be addressed- In addition to implementing the recommendations included in this report, the problems of staff morale can be addressed by ongoing meetings between labor and management. Opportunities for hearing staff concerns and for staff involvement in reform efforts should be made available.
C-12 Public stigma and anomie in institutions should be attacked - Public education efforts should be used to address the problems of stigma associated with mental illness. Complaints and concerns of system-users should be heard.
D. Oversight
D-1 Monitor conditions annually - The government should establish a process for the regular monitoring of the quality of hospital services and compliance with professional standards. At a minimum, each hospital should be evaluated once a year by a team of qualified professionals, and the results of the evaluations should be made available to professional organizations, family and consumer groups, and the general public.
D-2 Establish human rights committees - Each hospital should establish a human rights committee with broad representation not only from mental health professionals but from family, consumer and other advocacy organizations, to monitor compliance with human rights institutions. At a minimum, these committees should have access to information regarding the deaths of patients, reports of abuse or neglect, the use of physical and chemical restraints and seclusion, and complaints filed by patients or family members concerning the quality of care.
D-3 Support consumer and family advocates - The government should provide financial support to foster the development of consumer and family organizations to serve as advocates for a high quality of psychiatric and mental retardation services available in the least restrictive environment. In other countries, the families of people with mental retardation have been particularly effective advocates.
E. Recommendations to Advocates
E-1 Bring together a broad base of constituents for reform - There are many individuals and groups interested in changing mental health care. They need to be orga nized, perhaps with a new coalition of family groups, community providers, professionals (e.g. psychiatrists), human rights advocates, and others. Through this coalition, mental health can be made a human rights issue.
In other countries, reform has only taken place with leadership from profession als, government leaders and constituents, so an effort should be made to bring everyone into the reform process and assure that they play an active role in it.
E-2 Re-establish momentum around the 1985-86 National Program for Mental Health, which called for the creation of community-based services - In the mid-1980s, the National Program energized a broad array of constituents. By drawing on that plan and the experience of the people who put it together, some of the previous momentum for reform can be recaptured.
E-3 Educate the public about conditions in institutions and about the existence of alternatives to institutions - Advocates can instigate change by playing a role in public education. Priority should be placed on educating the public about conditions in institutions and about the existence of alternatives to hospitalization.
The international community should press for the enforcement of international human rights law:
E-4 The United Nations Special Rapporteur on the Equalization of Opportunities for Persons with Disabilities should evaluate the conditions of people with mental disabilities in Uruguay and Uruguay's efforts to create services and programs that will provide people with mental disabilities the full opportunity to live and work community.
The Special Rapporteur should provide technical assistance to Uruguay to create service programs in the community and should help raise international financial support for the development of such programs.
E-5 The United Nations Human Rights Committee should require Uruguay to report on the rights of people with mental disabilities under the ICCPR.
E-6 The United Nations Connnittee on Economic, Social, and Cultural Rights should require Uruguay to report on the rights of people with mental disabilities under the ICESCR.
Supplemental Bibliography
During discussions with mental health service providers in Uruguay, members of the MDRI team referred to a number of documents regarding psychiatric treatment and cross cultural issues in psychiatry. This material will provide a useful background to practitioners responding to issues raised in this report. Copies of the unpublished materials cited below are available through MORI, Washington College of Law, American University, 4400 Massachusetts Ave. NW, Washington, D.C. 20016-8084, United States of America (please send $5.00 to cover the cost of copying and postage). Copies may also be available through IELSUR in Montevideo, Uruguay.
Agency for Health Care Policy and Research, Public Health Service, United States Department of Health and Human Services, Depression in Primary Care: Treatment of Major Depression, 2 CLINICAL PRACTICE GUIDELINE (1993) (publication no. 93-0551).
- Depression in Primary Care: Detection, Diagnosis, and Treatment, CLINICAL PRACTICE GUIDELINE: QUICK REFERENCE GUIDE FOR CLINICIANS (1993) (publication no. 93-0552).
- Depression in Primary Care: Depression is a Treatable Illness, CLINICAL PRACTICE GUIDELINE: A PATIENT'S GUIDE (1993) (publication no. 93-0553).
- Depression in Primary Care: Detection and Diagnosis, 1 CLINICAL PRACTICE GUIDELINE (1993) (publication no. 93-0550).
American Psychiatric Association, Practice Guidelines for Major Depressive Disorder in Adults, 150 AM. J. PSYCHIATRY (Supplement, April 1993).
Febrega, Jr., Horacio, Hispanic Mental Health Research: A Case for Cultural Psychiatry, 12 HISPANIC JOURNAL OF BEHAVIORAL SCIENCES 339 (1990).
Mezzich, Juan Emique, Ruiz, Pedro, and Munoz, Rodrigo A., Delivering Mental Health Services to Hispanic Americans: Clinical, Educational and Research Perspectives (paper presented at the Center for Mental Health Services Conference on Hispanic Mental Health Care, December 2-4, 1993).
Rogler, Lloyd H., Cortes, Dharma E., Help-Seeking Pathways: A Unifying Concept in Mental Health Care, 150 AM. J. PSYCHIATRY 554 (1993).
South Bronx Mental Health Council, Inc., Clozapine Protocol (unpublished, August 1994).
- Controlled Substances Procedure (unpublished, August 1994).
- Directives for the Prevention and Treatment of Tardive Dyskinesia (unpublished, August 1994).
- General Protocol for all Patients on Psychotropic Medication (unpublished, August
1994). - Laboratory Procedure to be Followed with Patients that are on Psychotropic Medication (unpublished, August 1994).
- Medication Policy (unpublished, August 1994).
- Protocols for Patients on Psychotropic Medications (unpublished, August 1994).
- Protocol for the Use of Lithium Carbonate (unpublished, August 1995).
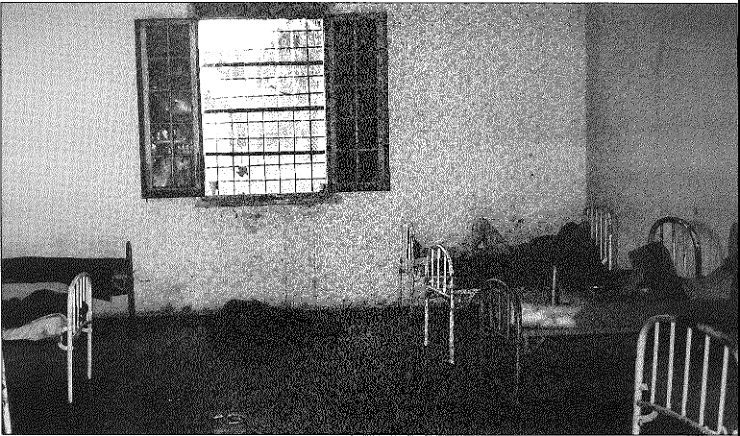
Security ward, Colonia Etcbepare - This is a locked, residential area of the Colonia Etchepare Security ward, where forty men reside. Any patient at Colonia Etchepare may be transferred to the security ward at the discretion of Colonia authorities. Toilets sinks were flooded at the time of the MDRI team's visit to the security ward, and overflow spilled or was tracked into halls and residential areas. Lacking any form of organized activity, many people spend their day in bed. A number of patients were observed sleeping or lying on the floor, some without clothes.
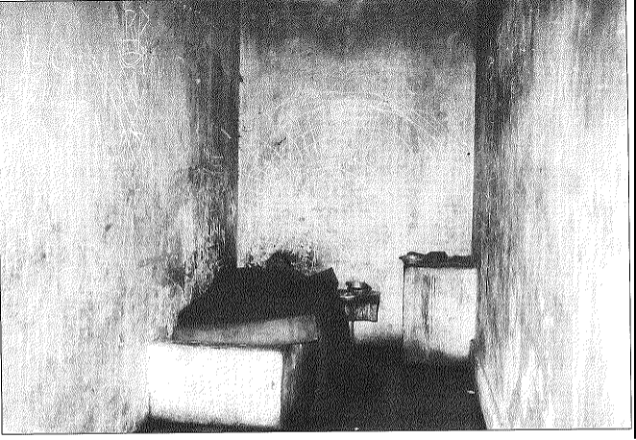
Seclusion room, security ward, Colonia Etchepare - This seclusion room is 1.8 by 3 meters, without natural light, and there is a small slit in the door for food. There is no sink and only a hole in the ground for a toilet, which must be flushed from the outside. Ward staff report that they may place a person in seclusion for one or two days without a physicians order. People are commonly kept in seclusion for a week, according to ward staff, but alcoholics are occasionally held in seclusion for forty-five days to "dry out." Authorities at Colonia Etchepare say that seclusion is not often used in Colonia Etchepare, except in the security ward. At the time of the MDRJ visit, no one was locked in the seclusion room. The individual pictured above renortedlv lived in the unlocked room on his own initiative.
